Father Martin’s Symptoms of Alcoholism
Father Joseph Martin's comprehensive symptom framework for alcoholism, developed decades before the modern DSM-5, demonstrates remarkable prescience in identifying the core features that would later become the official diagnostic criteria for Alcohol Use Disorder. His work essentially provided a detailed, experiential roadmap of how addiction manifests in real life, which closely parallels the clinical criteria psychiatrists use today.

1. DSM-5: "Alcohol taken in larger amounts or over longer periods than intended"
Father Martin's Parallel: "Loss of Control" - drinking more than intended
Martin's detailed exploration of this symptom captured the psychological torment of repeatedly breaking promises to oneself about consumption limits. He understood that this wasn't moral failure but neurological hijacking - the brain's reward system demanding more alcohol than conscious intention could control. His framework explained how someone could genuinely intend to have "just one drink" yet find themselves consuming far more, revealing the fundamental loss of voluntary control that defines addiction.
2. DSM-5: "Persistent desire or unsuccessful efforts to cut down or control alcohol use"
Father Martin's Parallel: "Change the Patterns" - switching brands, substances, designated days, suppliers
Martin's insight into pattern manipulation was revolutionary because it revealed how the addicted mind seeks to solve alcoholism through everything except stopping drinking. He recognized that elaborate schemes to control consumption - switching from liquor to beer, only drinking weekends, rotating suppliers - represented sophisticated denial mechanisms. These pattern changes provided the illusion of control while avoiding the fundamental solution: abstinence.
3. DSM-5: "Great deal of time spent obtaining, using, or recovering from alcohol"
Father Martin's Parallel: "Drinking becomes a full-time job" and "Protect the supply"
Martin understood that advanced alcoholism transforms from recreational activity to full-time occupation. His description of supply protection revealed how enormous mental and practical resources become devoted to ensuring alcohol access. The planning, procurement, concealment, and consumption of alcohol - along with recovery from its effects - eventually consumes entire days, leaving little time or energy for meaningful life activities.
4. DSM-5: "Craving or strong desire to use alcohol"
Father Martin's Parallel: "Racing thoughts about next use" and "Need to get back to a certain level"
Martin's framework captured how alcohol preoccupation colonizes mental space, creating obsessive planning and calculation around consumption. His insight about needing to reach a "certain level" revealed how addiction creates a physiological baseline where sobriety feels abnormal. The racing thoughts he described - constant planning around procurement and consumption - demonstrated how craving manifests as mental obsession that interferes with normal cognitive functioning.
5. DSM-5: "Failure to fulfill major role obligations due to alcohol use"
Father Martin's Parallel: "Past due bills," "Past due obligations," and "Other things become less important"
Martin's detailed exploration of priority inversion showed how alcohol gradually assumes emergency-level importance, displacing responsibilities that once mattered. His examples of unpaid bills, missed obligations, and neglected relationships revealed how addiction systematically reorganizes life priorities around alcohol access and consumption, often without conscious awareness of this fundamental shift.
6. DSM-5: "Continued use despite social or interpersonal problems"
Father Martin's Parallel: "Loss of friends/family" and "Anti-social behavior"
Martin recognized that alcoholism creates a vicious cycle where drinking causes relationship problems, but the pain of damaged relationships drives more drinking. His framework explained how isolation becomes both consequence and cause of continued alcohol use. The progressive social withdrawal he described - from stopping getting invited places to complete disconnection from community - mapped the trajectory of social deterioration that accompanies advancing addiction.
7. DSM-5: "Important activities given up or reduced because of alcohol use"
Father Martin's Parallel: "The addiction dictates the places we go and who we go there with"
Martin's insight that addiction controls geographic and social choices revealed how alcoholism systematically eliminates activities incompatible with drinking. His framework showed how hobbies, career opportunities, family activities, and personal interests are gradually abandoned in favor of alcohol-centered living, often without conscious recognition of these losses until they become irreversible.
8. DSM-5: "Use in physically hazardous situations"
Father Martin's Parallel: "Accidents or injuries while under the influence"
Martin understood that alcohol impairs judgment about risk assessment, leading to dangerous behaviors that seem incomprehensible in retrospect. His framework captured how intoxication creates false confidence while simultaneously impairing the very faculties needed to assess danger accurately. The accidents and injuries he described often serve as wake-up calls that reveal how seriously alcohol has compromised safety judgment.
9. DSM-5: "Continued use despite physical or psychological problems"
Father Martin's Parallel: "Medical problems," "Hospitals or medical support," and "Nameless fears and anxiety"
Martin's comprehensive exploration of medical consequences revealed how alcoholism creates a tragic paradox: the substance used to cope with problems actually creates far more serious problems. His framework included both obvious physical damage (liver disease, heart problems) and psychological symptoms (anxiety, depression) that persist despite clear evidence that alcohol is causing these very problems.
10. DSM-5: "Tolerance - need for increased amounts to achieve desired effect"
Father Martin's Parallel: "Eye opener" and "Functioning better under the influence"
Martin's eye opener concept captured how tolerance creates the need for alcohol to achieve what feels like normal functioning. His insight that this "doesn't have to be in the morning" was revolutionary - he recognized that tolerance creates round-the-clock dependence where alcohol becomes necessary for basic daily functioning regardless of time or circumstances. The belief in functioning better under the influence reflects how tolerance makes sobriety feel like impairment.
11. DSM-5: "Withdrawal symptoms or alcohol taken to relieve/avoid withdrawal"
Father Martin's Parallel: "Tremors or shakes," "Lack of body control," and "Need to get back to a certain level"
Martin's detailed description of withdrawal symptoms revealed how physical dependence transforms alcohol from choice to necessity. His framework captured both obvious symptoms (tremors, shakes) and subtle signs (anxiety, inability to function normally) that drive continued consumption to prevent withdrawal distress. The "certain level" concept showed how maintenance drinking develops to avoid withdrawal rather than achieve intoxication.
Father Martin's Additional Insights Beyond DSM-5
While Father Martin's framework paralleled future DSM-5 criteria remarkably well, he also provided insights that enriched understanding beyond clinical diagnosis:
The Alibi System revealed the sophisticated psychological defense mechanisms that protect continued drinking through elaborate justification and blame deflection. This insight helped explain why logical arguments about alcohol's consequences often fail to motivate change.
Gulping and Sneaking captured the behavioral changes that signal transition from social to dependent drinking. These behaviors often precede more obvious symptoms and can serve as early warning signs.
Blackouts and Brownouts provided crucial evidence of alcohol's neurotoxic effects while also explaining why consequences often fail to modify behavior - if you can't remember negative consequences, they can't inform future decisions.
Binges and Benders revealed that alcoholism doesn't always manifest as daily drinking but can involve devastating periodic episodes that are equally serious and dangerous.
The Therapeutic Value of Father Martin's Framework
Father Martin's approach was particularly powerful because it:
Normalized Symptoms: By presenting these behaviors as predictable symptoms rather than moral failings, he reduced shame and defensiveness that often prevent treatment seeking.
Provided Recognition Points: His detailed descriptions helped people recognize their own experiences, often for the first time seeing their struggles as part of a recognizable medical condition.
Explained Progression: His framework showed how symptoms typically develop and worsen over time, helping people understand they were dealing with a progressive disease requiring intervention.
Offered Hope: By framing these symptoms as disease manifestations rather than character defects, he implied they could be treated and recovery was possible.
Educated Families: His descriptions helped family members understand that bewildering and hurtful behaviors were symptoms of illness rather than evidence that their loved one no longer cared about them.
The Bridge Between Experience and Science
Father Martin's work represents a crucial bridge between lived experience and clinical science. His framework emerged from decades of observing and treating people with alcoholism, providing rich phenomenological descriptions that captured the full human experience of addiction. When researchers later developed the DSM-5 criteria, they were essentially codifying and systematizing insights that practitioners like Father Martin had already identified through careful observation and clinical experience.
This convergence between experiential wisdom and scientific research validates both approaches: Father Martin's observations were scientifically accurate, while the DSM-5 criteria capture real-world experiences that people with alcohol use disorders actually live through.
The enduring value of Father Martin's work lies not just in its diagnostic accuracy, but in its compassionate, detailed exploration of how alcoholism actually manifests in daily life. While the DSM-5 provides essential clinical criteria for diagnosis, Father Martin's framework provides the human context that helps people recognize, understand, and ultimately address the complex reality of alcohol use disorder in all its manifestations.
His work reminds us that behind every clinical criterion lies a human story of struggle, loss, and ultimately, the possibility of recovery through understanding, treatment, and hope.
The Neurological Foundation of Memory Loss:
Father Martin understood that blackouts weren't simply about drinking "too much" on occasion - they represented a specific type of brain dysfunction that occurs when alcohol concentrations interfere with the hippocampus, the brain's memory formation center. This isn't the same as passing out or losing consciousness. During a blackout, you remain awake, walking, talking, and seemingly participating in life, but your brain has stopped recording experiences into long-term memory.
The distinction between blackouts and brownouts is crucial. Complete blackouts leave absolutely no memory traces - it's as if those hours simply didn't exist in your personal history. Brownouts, or fragmentary blackouts, leave scattered pieces of memory that feel like trying to remember a dream. You might recall standing in a kitchen but not how you got there, or remember laughing but not what was funny.
"Piecing Together the Evening" - The Detective Work of Lost Time:
This phrase captures one of the most disturbing aspects of memory loss from drinking. You wake up and realize that significant portions of your life are missing, and you must become a detective investigating your own actions. This process involves calling friends, checking your phone for clues, looking for physical evidence of where you went and what you did.
The "piecing together" process often reveals disturbing information. You might discover you drove somewhere with no memory of the trip, spent large amounts of money, or behaved in ways completely contrary to your values and personality. Friends might tell you about conversations you had, jokes you made, or arguments you started that exist in their memory but not yours.
This detective work becomes increasingly important as the consequences of blackout behavior accumulate. You need to know if you made commitments you can't remember, damaged relationships, or put yourself in dangerous situations. The anxiety of not knowing what you might have done can be overwhelming, especially when others seem reluctant to fill in the missing pieces.
Making Phone Calls You Can't Remember:
A particularly revealing type of blackout behavior. Operating a phone requires complex cognitive functions - remembering numbers, navigating through contacts, carrying on conversations, and responding appropriately to others. The fact that you can perform these sophisticated tasks while being unable to form memories demonstrates how alcohol can selectively impair certain brain functions while leaving others temporarily intact.
These mysterious phone calls often have serious consequences. You might call an ex-partner and reopen old wounds, contact your boss and say inappropriate things, make promises to friends you can't keep, or reveal personal information you normally wouldn't share. Family members might receive late-night calls where you repeat the same stories or concerns multiple times, not remembering that you've already called them earlier.
The technology trail left by these calls can be particularly revealing and embarrassing. Your phone records, text messages, and social media posts become evidence of activities you can't remember. You might wake up to find sent messages that sound like they were written by someone else, or discover you've made plans you have no recollection of making.
Having to Be Reminded of Things You Said or Did:
This symptom reveals how blackouts affect not just your memory, but your relationships and social functioning. When others have to constantly remind you of your own words and actions, it creates a profound imbalance in relationships. Friends and family members become reluctant historians of your life, holding memories that belong to you but that you can't access.
These reminders often come with emotional weight. Someone might say, "Don't you remember? You promised to help me move this weekend," or "You told me last night that you were thinking about quitting your job." Each reminder reveals the gap between your blackout self and your sober self, and the disconnect can be deeply disturbing.
The pattern of needing reminders also creates relationship strain. People close to you may become frustrated with having to repeatedly explain things you should remember. They might start to question whether you're genuinely unable to remember or simply claiming not to remember to avoid responsibility for your actions.
The Progressive Nature of Memory Impairment:
Father Martin observed that blackouts typically don't occur during someone's first drinking experiences. They usually appear after tolerance has developed and drinking patterns have intensified. Early in someone's drinking career, they might experience partial memory loss or haziness about events. As drinking progresses, these memory gaps become more frequent and complete.
The progression often follows a predictable pattern: first, you might not remember the end of evenings; then entire conversations disappear; eventually, you might lose hours at a time. Some people reach a point where they can function through complex activities - driving across town, having dinner at a restaurant, attending social events - with no memory formation whatsoever.
Functional Blackouts vs. Obvious Intoxication:
One of Father Martin's key insights was that blackouts don't always correspond with obvious signs of intoxication. You might appear relatively sober to others while experiencing complete memory loss. This "functional" drinking during blackouts can be particularly dangerous because others don't realize the extent of your impairment and may treat you as if you're making conscious, memorable decisions.
During functional blackouts, you might drive (often successfully, which reinforces the dangerous belief that you're "fine"), make important decisions, sign documents, or engage in intimate relationships without the capacity to form memories of these experiences. The lack of obvious impairment means others don't intervene or take protective measures.
The Psychological Impact of Lost Time:
Beyond the immediate safety concerns, the psychological impact of regular blackouts can be devastating. Large portions of your life become inaccessible to you, creating a sense of discontinuity in your personal narrative. You might feel like you're living someone else's life or that there are multiple versions of yourself operating without your knowledge or consent.
The uncertainty can create persistent anxiety. If you can't remember what you did last night, how can you be sure you didn't hurt someone, damage property, or make decisions that will have serious consequences? This anxiety often drives more drinking as a way to cope with the stress of not knowing what your "other self" might have done.
The Denial and Minimization Factor:
Father Martin noted that people experiencing blackouts often minimize their significance or deny they're happening. You might tell yourself that everyone drinks too much sometimes and forgets things, or that you're just tired and not thinking clearly. The brain's remarkable ability to fill in memory gaps with plausible scenarios can make it easier to dismiss blackouts as unimportant.
This denial is often reinforced by the fact that life continues despite the memory loss. You wake up in your own bed, your car is in the driveway, and there are no obvious disasters, so the blackout seems less serious than it actually was. However, the absence of immediate catastrophic consequences doesn't negate the serious underlying brain dysfunction that blackouts represent.
Father Martin's focus on these memory-related symptoms was crucial because they often precede the more obvious signs of late-stage alcoholism. Recognizing blackouts and brownouts as serious warning signs, rather than occasional inconveniences, can be a critical step in acknowledging the need for help before drinking causes irreversible damage to health, relationships, and life circumstances.

Gulping - Drinking Quickly to Reach a Certain Level:
This behavior reflects a fundamental shift in the relationship with alcohol. Unlike social drinkers who sip and savor their drinks, people developing alcohol dependency often drink rapidly with a specific goal in mind - to achieve a particular feeling or blood alcohol level as quickly as possible.
Gulping serves several purposes for someone with developing alcoholism. First, it's about efficiency - getting the desired effect without prolonged social interaction or scrutiny from others. You might down two drinks quickly while others are still working on their first, then switch to nursing drinks to appear normal. This rapid consumption also helps avoid the anxiety or discomfort that comes from being sober in social situations.
The "certain level" aspect is particularly telling. This isn't about enjoying the taste or social aspects of drinking - it's about reaching a specific state of intoxication where you feel "right" or "normal." You might have a mental target, knowing you need three drinks quickly to feel comfortable at a party, or downing drinks before going out so you're already at your desired level when you arrive.
This pattern often develops because tolerance has increased. What once required one drink to feel relaxed now requires three or four, so drinking quickly becomes a practical necessity to achieve the same effect within a socially acceptable timeframe.
Sneaking and Hiding Your Supply:
Secretive drinking behaviors emerge from shame, fear of judgment, and the need to maintain a facade of control. These behaviors often develop gradually and can become quite elaborate over time.
Hiding alcohol supplies might start innocently - keeping a bottle in your desk drawer for "after work stress relief" or stashing beer in the garage so your spouse doesn't see how much you're drinking. However, these behaviors typically escalate into more complex deception systems. You might hide bottles in multiple locations throughout your home, car, or workplace, ensuring you always have access when needed.
The secrecy serves multiple psychological functions. It allows you to maintain the illusion that your drinking isn't problematic - after all, if it were really a problem, why would you be able to hide it so effectively? It also protects against confrontation from family members or friends who might express concern about your consumption levels.
Multiple Locations - Creating a Supply Network:
Having alcohol stashed in various locations represents a sophisticated level of planning that indicates drinking has become a central organizing principle in your life. This isn't casual drinking - it's strategic positioning to ensure access regardless of circumstances.
Multiple locations might include your home office, bedroom, basement, garage, car glove compartment, workplace, gym bag, or even outdoor hiding spots. Each location serves a specific purpose: the workplace stash for dealing with job stress, the car supply for drinking before social events, the bedroom bottle for nighttime consumption without disturbing family members.
This behavior also reflects anticipatory anxiety about being without alcohol. The fear of being caught without a drink when you need one becomes so overwhelming that you create redundant supply systems. You might buy alcohol at different stores to avoid judgment from clerks, or purchase in smaller quantities more frequently to make your consumption appear more moderate.
The Escalation Pattern:
These behaviors rarely appear overnight. They typically develop progressively as tolerance increases and social drinking transforms into dependency. You might start by drinking a bit faster than others, then progress to pre-drinking before social events, then to keeping a "backup" bottle at home, eventually evolving into elaborate concealment systems.
Psychological Implications:
The need to gulp and sneak reveals the internal conflict between wanting to drink and knowing that your consumption patterns are problematic. The gulping addresses the physical need for alcohol's effects, while the sneaking addresses the social and psychological need to appear normal and in control.
These behaviors also indicate that alcohol has begun to take precedence over honesty in relationships. The energy and mental resources devoted to hiding consumption, remembering where supplies are hidden, and maintaining deceptive behaviors represents a significant shift in priorities and values.
Warning Signs for Loved Ones:
Family members and friends might notice indirect evidence of these behaviors: empty bottles appearing in unusual places, rapid consumption when alcohol is available, mysterious disappearances during social events (often to access hidden supplies), or finding alcohol in unexpected locations. The person might also become defensive or agitated when their drinking patterns are questioned, or show signs of relief when they know alcohol will be available at upcoming events.
Father Martin's identification of these patterns was groundbreaking because it moved beyond simply measuring quantity of alcohol consumed to examining the behaviors and motivations surrounding drinking. These sneaking and gulping behaviors often precede the more obvious signs of alcoholism, making them valuable early warning indicators for both the individual and their loved ones.
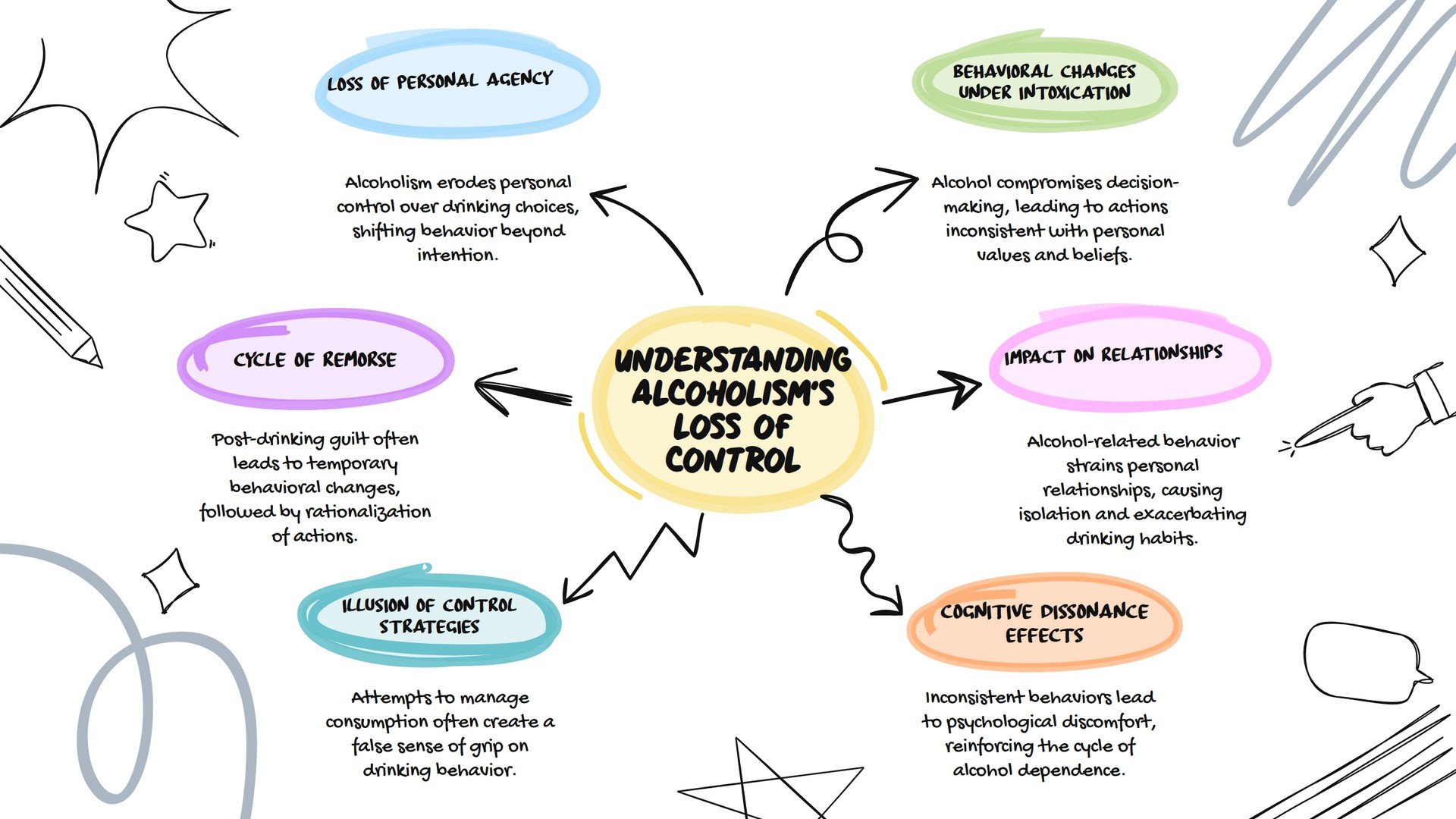
The Fundamental Nature of Control Loss:
Father Joseph Martin's identification of "loss of control" as a cardinal symptom of alcoholism was groundbreaking because it moved beyond measuring how much someone drinks to examining their relationship with alcohol and their ability to govern their own behavior. This symptom strikes at the heart of what distinguishes alcoholism from heavy drinking - the erosion of personal agency and self-determination.
Loss of control in alcoholism isn't simply about making poor decisions while intoxicated. It represents a fundamental breakdown in the brain's executive function - the complex system that governs planning, decision-making, impulse control, and behavioral regulation. Father Martin understood that this wasn't a moral failing or lack of willpower, but a neurological consequence of how alcohol affects the brain's reward and control systems.
The loss of control manifests in two distinct but interconnected ways: the inability to control consumption once drinking begins, and the inability to control behavior while under the influence. Both aspects reflect how alcohol hijacks the brain's normal regulatory mechanisms, creating a cycle where the substance that promises to solve problems actually creates more severe ones.
Drinking More Than Intended - The Consumption Control Failure:
The question "Have you ever drunk more than you intended to?" appears deceptively simple, but it reveals a profound shift in the relationship with alcohol. For social drinkers, consumption is generally predictable and controllable. They can decide to have one drink and stop at one, or plan for two drinks and successfully limit themselves to that amount.
When alcoholism develops, this predictability disappears. You might go to happy hour planning to have one beer and find yourself closing down the bar hours later. You might buy a bottle of wine intending to have a glass with dinner and discover the entire bottle is empty by bedtime. The gap between intention and reality becomes increasingly wide and unpredictable.
This loss of consumption control often follows a characteristic pattern. Early in the development of alcoholism, the overage might be modest - planning for two drinks but having three or four. As the condition progresses, the gap widens dramatically. You might intend to have a couple of drinks and end up in a multi-day bender, or plan to drink only on weekends but find yourself drinking daily.
The psychological impact of this pattern is particularly devastating because it directly contradicts your self-image as someone in control of their choices. Each episode of drinking more than intended becomes evidence that your willpower and decision-making abilities are unreliable. This often leads to increased shame, self-blame, and paradoxically, more drinking to cope with these negative feelings.
The broken promises to yourself accumulate over time. You might promise to limit yourself to beer instead of hard liquor, only to find yourself drinking vodka by the end of the evening. You might decide to drink only at social events, then find yourself drinking alone at home. Each broken commitment to yourself reinforces the sense that you cannot trust your own intentions or rely on your ability to control your consumption.
Behavioral Control Failure - Actions Contrary to Character:
The second aspect of Father Martin's loss of control symptom - saying or doing things you wouldn't do sober - reveals how alcohol systematically dismantles the inhibitory mechanisms that normally govern behavior. This isn't just about making mistakes; it's about acting in ways that are fundamentally inconsistent with your values, personality, and moral framework.
Alcohol affects the prefrontal cortex, the brain region responsible for executive decision-making, impulse control, and social judgment. As this area becomes impaired, the normal filters that prevent inappropriate behavior become less effective. The result is that thoughts, feelings, and impulses that would normally remain private or controlled can manifest as actions and words.
These behavioral changes often follow predictable patterns that reflect underlying tensions and suppressed emotions. A normally quiet person might become loud and aggressive. Someone who is typically diplomatic might become brutally honest or cruel. A person who values discretion might share intimate details of their life with strangers. The alcohol doesn't create these impulses - it removes the normal barriers that keep them in check.
The Spectrum of Behavioral Loss:
The behaviors that emerge during intoxication can range from mildly embarrassing to seriously destructive. On the milder end, you might find yourself oversharing personal information, making inappropriate jokes, or being more flirtatious than usual. These actions might cause embarrassment but don't typically have lasting consequences.
As the loss of control deepens, the behaviors become more serious. You might engage in verbal arguments that damage relationships, make financial decisions you can't afford, drive when you know you shouldn't, or engage in sexual behavior that contradicts your normal judgment. These actions can have lasting consequences for relationships, career, finances, and legal standing.
At the severe end of the spectrum, alcohol-induced behavior can become dangerous or criminal. This might include physical altercations, property damage, driving under the influence, or other actions that put yourself and others at serious risk. The person who emerges during these episodes can seem like a stranger to family and friends - and often to yourself when you learn about your actions later.
The Dr. Jekyll and Mr. Hyde Phenomenon:
Father Martin often referenced the stark personality changes that can occur with drinking, comparing them to the classic literary transformation of Dr. Jekyll and Mr. Hyde. This metaphor captures how alcohol can reveal or unleash aspects of personality that seem completely foreign to the sober individual.
Family members frequently describe feeling like they're living with two different people - the sober person they love and respect, and the intoxicated person they fear or don't recognize. This duality creates tremendous confusion and stress in relationships because it's difficult to know which version of the person is "real" or which one to expect in any given situation.
The intoxicated persona often acts on impulses and emotions that the sober person works hard to manage or suppress. Years of accumulated resentments might pour out in angry tirades. Sexual desires that are normally controlled might lead to infidelity or inappropriate advances. Financial anxieties might result in reckless spending or gambling.
The Remorse and Rationalization Cycle:
Father Martin observed that the loss of control typically follows a predictable emotional cycle. After episodes of drinking more than intended or behaving inappropriately, there's usually a period of intense remorse and self-recrimination. You might feel horrified by your actions, ashamed of your lack of control, and determined to prevent similar episodes in the future.
This remorse often leads to temporary behavior changes - you might avoid drinking for days or weeks, apologize profusely to people you've hurt, or make grand promises about changing your relationship with alcohol. However, without addressing the underlying neurological and psychological factors driving the loss of control, these periods of abstinence or moderation are typically temporary.
As time passes and the immediate consequences fade, rationalization often sets in. You might minimize the severity of your actions, blame external circumstances, or convince yourself that you can prevent similar episodes through willpower alone. This rationalization process sets the stage for the cycle to repeat, often with escalating severity.
The Erosion of Personal Values and Identity:
One of the most disturbing aspects of alcohol-induced loss of control is how it can cause you to act in ways that directly contradict your core values and beliefs. A person who prides themselves on honesty might become deceptive. Someone who values family above all else might neglect or hurt their loved ones. A professional who has worked hard to build their reputation might engage in career-damaging behavior.
These value violations create a profound sense of cognitive dissonance - the psychological discomfort that comes from acting in ways that contradict your beliefs about yourself. This dissonance often drives increased drinking as a way to escape the uncomfortable reality of who you become when intoxicated.
Over time, the repeated pattern of value violations can lead to a fundamental erosion of self-respect and identity. You might begin to question whether your sober values are authentic or whether the intoxicated version represents your "true" self. This identity confusion can deepen the psychological dependence on alcohol and make recovery more challenging.
The Illusion of Control and Its Consequences:
Many people experiencing loss of control attempt to manage it through various strategies - switching types of alcohol, only drinking at certain times or places, or implementing elaborate rules about when and how much to drink. Father Martin recognized that these attempts often create an illusion of control while the underlying problem continues to worsen.
The failure of these control strategies often leads to increased shame and self-blame. You might conclude that you lack willpower or moral character, rather than recognizing that you're dealing with a medical condition that affects brain function. This self-blame can become a barrier to seeking help, as you might believe that you should be able to solve the problem through determination alone.
Professional and Social Consequences:
The loss of control symptoms often create ripple effects that extend far beyond the immediate drinking episodes. Professional relationships might suffer if colleagues witness inappropriate behavior at work events. Friendships can be damaged by broken commitments or hurtful words spoken during intoxication. Family relationships often bear the greatest burden, as loved ones must cope with the unpredictability and potential danger of someone whose behavior becomes unreliable when drinking.
The cumulative impact of these damaged relationships can create a social isolation that paradoxically increases the likelihood of continued drinking. As natural support systems erode due to alcohol-related behavior, drinking might become the primary coping mechanism for dealing with loneliness and social consequences.
Father Martin's insight into loss of control as a cardinal symptom of alcoholism was revolutionary because it helped people understand that their struggles with alcohol weren't simply a matter of making better choices or trying harder to control themselves. By recognizing loss of control as a symptom of a progressive medical condition rather than a moral failing, he opened the door for people to seek appropriate treatment rather than continuing to blame themselves for their inability to drink "normally."
The Psychological Architecture of the Alibi System:
Father Martin's identification of the "alibi system" as a fundamental symptom of alcoholism revealed one of the most sophisticated psychological mechanisms that develops alongside addiction. The alibi system represents a complex network of justifications, rationalizations, and blame deflection that serves to protect continued drinking while maintaining the illusion that the drinking is reasonable, necessary, or someone else's fault.
Father Martin's identification of the "alibi system" as a fundamental symptom of alcoholism revealed one of the most sophisticated psychological mechanisms that develops alongside addiction. The alibi system represents a complex network of justifications, rationalizations, and blame deflection that serves to protect continued drinking while maintaining the illusion that the drinking is reasonable, necessary, or someone else's fault.
The alibi system doesn't develop overnight - it evolves gradually as a protective psychological mechanism that allows continued drinking while avoiding the painful reality of loss of control. Father Martin understood that this wasn't simply lying or making excuses; it's a comprehensive cognitive framework that actually changes how someone perceives reality, causation, and personal responsibility.
This system serves multiple psychological functions simultaneously. It protects the ego from acknowledging the extent of the drinking problem, provides rational-sounding justifications for continued alcohol use, shifts responsibility away from personal choices, and maintains the belief that drinking is a solution rather than the primary problem. The alibi system becomes so sophisticated and automatic that the person often believes their own justifications completely.
Creating Reasons to Drink - The Manufactured Necessity:
The question "Did you create reasons to drink?" exposes how alcoholism transforms drinking from a choice into a perceived necessity. As dependence develops, the brain begins to prioritize alcohol consumption above other activities, but the conscious mind needs acceptable explanations for this prioritization.
These manufactured reasons often start innocuously. You might decide you need a drink to "unwind" after work, celebrate small victories, cope with minor stresses, or enhance social situations. Initially, these reasons might seem legitimate and socially acceptable. However, as the disease progresses, the reasons become increasingly elaborate and divorced from reality.
The creation of drinking reasons often follows predictable patterns. Stress becomes the universal justification - any difficulty at work, relationship tension, financial pressure, or even positive events like promotions or anniversaries become "reasons" why drinking is not only acceptable but necessary. The stress doesn't have to be significant; minor inconveniences can be elevated to crisis status to justify alcohol consumption.
Weather becomes another reliable source of drinking justifications. It's too hot, too cold, too rainy, too sunny, or just the right temperature for drinking. Holidays and celebrations expand beyond traditional occasions to include personal anniversaries, the end of difficult weeks, or even the simple fact that it's Friday. The calendar becomes a constellation of drinking opportunities, each with its own manufactured significance.
Social obligations transform into drinking necessities. Business dinners "require" alcohol to facilitate networking. Family gatherings become unbearable without liquid courage. Even activities that traditionally don't involve drinking - children's sporting events, afternoon shopping trips, or casual coffee meetings - can be reframed as situations where alcohol consumption is appropriate or helpful.
The Blame Deflection Mechanism:
The second component of Father Martin's alibi system - blaming others - represents a sophisticated psychological defense that protects the drinking behavior by attributing its necessity to external forces beyond personal control. This blame deflection serves to maintain the illusion that drinking is a reasonable response to unreasonable circumstances created by other people.
Spouses and family members often become primary targets of this blame system. Your drinking might be attributed to your partner's nagging, lack of understanding, or failure to provide adequate support. Children's behavior, whether good or bad, can be used to justify drinking - celebrating their achievements or coping with their problems. Extended family dynamics, in-laws, or family obligations become sources of stress that "require" alcohol to manage.
Workplace blame is equally common and sophisticated. Difficult bosses, unreasonable deadlines, office politics, demanding clients, or incompetent colleagues all become justifications for after-work drinking. Even positive work situations can be blamed - success creates pressure that needs to be relieved with alcohol, while failures create disappointment that needs to be numbed with drinking.
Friends and social circles can also be incorporated into the blame system. You might drink because your friends don't understand you, because they pressure you to drink, or because they don't provide enough social stimulation without alcohol. Conversely, you might blame them for not drinking enough to keep up with your consumption levels, making you feel isolated or different.
Societal and political issues provide another layer of blame deflection. Economic conditions, political developments, social problems, or even global events can be cited as justifications for drinking. The state of the world becomes personally overwhelming, requiring alcohol as a coping mechanism for circumstances completely beyond individual control.
The Excuse Manufacturing Process:
The third element of the alibi system - finding excuses and reasons - involves the active creation of elaborate justifications that transform drinking from a personal choice into an inevitable response to circumstances. This process becomes increasingly creative and complex as simpler excuses lose their effectiveness or believability.
Medical excuses often feature prominently in this system. Minor aches and pains become chronic conditions requiring alcohol for pain management. Insomnia necessitates drinking to sleep. Anxiety or depression symptoms, whether diagnosed or self-identified, become medical reasons for self-medication with alcohol. Even positive health developments can be twisted into drinking justifications - completing a workout "earns" celebratory drinks, or finishing a diet allows for alcohol rewards.
Financial excuses can work in multiple directions. Having money becomes a reason to celebrate with expensive alcohol, while lacking money creates stress that requires cheap alcohol to manage. Getting a raise justifies upgrading drinking habits, while financial struggles necessitate drinking to cope with economic pressure. Even saving money on other expenses can be reframed as creating a "budget" for alcohol purchases.
Social obligations provide rich material for excuse generation. Weddings, funerals, business events, family gatherings, or casual social meetings all become situations where not drinking would be rude, antisocial, or professionally damaging. The excuse system transforms alcohol consumption from a personal choice into a social necessity dictated by external expectations and obligations.
The Evolution and Sophistication of Alibis:
Father Martin observed that alibi systems become increasingly sophisticated over time as simpler justifications lose their effectiveness. Early in the development of alcoholism, basic excuses might suffice - drinking to relax after work or celebrate weekends. As tolerance develops and drinking increases, more elaborate justifications become necessary.
The evolution often follows a pattern from reactive to proactive excuse generation. Initially, excuses might be created after drinking episodes to explain or justify what has already occurred. As the system develops, excuses are generated in advance, creating a framework that pre-justifies future drinking. Eventually, the excuse system becomes so comprehensive that almost any situation can be interpreted as a valid reason for alcohol consumption.
Advanced alibi systems often incorporate elements of victimization and martyrdom. The person begins to see themselves as suffering uniquely difficult circumstances that others couldn't understand or handle without alcohol. This victimization narrative serves multiple functions - it justifies continued drinking, generates sympathy from others, and deflects criticism by positioning any questioning of drinking habits as additional persecution.
The Self-Fulfilling Prophecy Element:
One of the most insidious aspects of the alibi system is how it can actually create the problems it claims to address. When relationship difficulties are consistently blamed for drinking, the drinking behavior often creates additional relationship problems, which then serve as new justifications for continued alcohol use. Work stress blamed for drinking can lead to alcohol-related performance issues, creating genuine work problems that reinforce the original excuse.
This self-fulfilling prophecy aspect makes the alibi system particularly resistant to logical challenges. When someone points out that drinking might be causing rather than solving problems, the person can point to real difficulties in their life as evidence that their drinking is justified. The fact that alcohol might be contributing to or creating these problems becomes increasingly difficult to see through the lens of the established alibi system.
The Impact on Relationships and Communication:
The alibi system profoundly affects relationships because it makes honest communication about drinking nearly impossible. Family members and friends find themselves constantly having their concerns deflected back onto them as the "real" source of problems. Attempts to discuss drinking are reframed as nagging, lack of support, or failure to understand the legitimate stresses that necessitate alcohol use.
This dynamic creates a frustrating cycle for loved ones. They observe the destructive effects of drinking but find themselves positioned as the problem whenever they attempt to address it. The alibi system effectively shields the drinking behavior from examination by making anyone who questions it into part of the problem rather than part of the solution.
Spouses often find themselves walking on eggshells, afraid that any conflict or stress might be used as justification for drinking episodes. Children learn that their normal developmental challenges - school problems, social issues, or behavioral difficulties - might trigger parental drinking. The entire family system can become organized around avoiding situations that might feed into the alibi system.
The Professional and Social Consequences:
In professional settings, the alibi system can create significant problems while simultaneously providing explanations for declining performance. Workplace conflicts, missed deadlines, or poor decision-making can all be attributed to external stresses rather than alcohol-related impairment. This can delay recognition of alcohol problems and postpone necessary interventions.
Social relationships often suffer as friends and acquaintances tire of hearing elaborate justifications for drinking behavior. The constant need to explain, justify, and deflect blame can make social interactions exhausting for everyone involved. People may begin to avoid social contact or stop inviting the person to events, which then provides new material for the alibi system - social isolation becomes another reason why drinking is necessary.
The Barrier to Treatment and Recovery:
Father Martin recognized that the alibi system represents one of the most significant barriers to seeking treatment and achieving recovery. As long as drinking can be justified as a reasonable response to external circumstances, there's no reason to consider it a problem requiring professional help. The system provides a complete alternative explanation for all the negative consequences of drinking.
Even when problems become severe enough to consider treatment, the alibi system can interfere with recovery efforts. In therapy or support groups, energy that should be focused on addressing drinking behavior may instead be devoted to proving that the drinking is justified by circumstances. The habit of blame deflection and excuse generation can persist long after alcohol consumption stops, interfering with the honest self-assessment necessary for sustained recovery.
Breaking Through the Alibi System:
Father Martin's identification and articulation of the alibi system was therapeutic in itself because it helped people recognize these patterns in their own thinking. By naming and describing these mechanisms, he made it possible for individuals to step back and examine their own justification systems with greater objectivity.
The process of dismantling an alibi system often requires external help because the system is designed to be self-reinforcing and resistant to internal challenge. Professional counselors, support groups, and trusted friends or family members can provide the outside perspective necessary to identify and challenge the elaborate justifications that have become automatic and unconscious.
Recovery often involves developing new ways of understanding causation and personal responsibility. Instead of seeing drinking as a reasonable response to external stresses, people learn to recognize it as a primary problem that creates additional difficulties. This shift in perspective - from seeing alcohol as solution to seeing it as problem - represents a fundamental restructuring of the cognitive framework that supports the alibi system.
Father Martin's insight into the alibi system revealed how alcoholism affects not just behavior and physical health, but the very way people think about causation, responsibility, and reality. By understanding these psychological mechanisms, both individuals struggling with alcohol and their loved ones can better recognize when justifications have crossed the line from reasonable explanations into pathological defense systems that protect and perpetuate destructive drinking patterns.
Redefining the Eye Opener Beyond Morning Drinking:
Father Joseph Martin's identification of the "eye opener" as a symptom of alcoholism represents one of his most profound insights into how addiction fundamentally alters the body's biochemical equilibrium and the mind's perception of normal functioning. This symptom reveals the transition from drinking for pleasure or social reasons to drinking for physiological and psychological necessity - a shift that marks the progression from heavy drinking to true alcoholism.
Father Martin's crucial clarification that "this does not have to be in the morning" was revolutionary in addiction treatment because it expanded understanding beyond the stereotypical image of the morning drunk. Traditional concepts of eye openers focused on people who needed alcohol immediately upon waking to function, but Martin recognized that this symptom manifests across all times of day and in various circumstances.
The eye opener isn't defined by the clock - it's defined by the need for alcohol to achieve what feels like normal functioning, regardless of when that need arises. You might need a drink before a business meeting at 2 PM to feel confident and composed. You might require alcohol before family dinner to feel comfortable and sociable. The defining characteristic isn't the timing, but the sense that alcohol is necessary to restore you to a state where you can function at what feels like your optimal level.
This broader definition captures the reality of how modern alcoholism often develops. Many people maintain employment, family responsibilities, and social obligations while still experiencing the eye opener phenomenon. They might not drink in the morning, but they systematically use alcohol throughout the day to manage anxiety, enhance performance, or achieve emotional balance in various situations.
The Biochemical Foundation of Needing Restoration:
The concept of needing alcohol to be "restored to balance" reflects the profound biochemical changes that occur as alcoholism develops. The brain's neurotransmitter systems, particularly those involving GABA (which produces calm, relaxed feelings) and dopamine (associated with pleasure and motivation), become dependent on alcohol's presence to function normally.
In healthy individuals, the brain naturally produces the chemicals necessary for appropriate mood, anxiety levels, and cognitive function. However, chronic alcohol use causes the brain to reduce its natural production of these substances, relying instead on alcohol to provide the chemical balance necessary for normal functioning. This creates a state where sobriety doesn't feel normal - it feels deficient, anxious, and uncomfortable.
The "restoration to balance" isn't just psychological - it's physiological. Without alcohol, you might experience subtle but persistent symptoms: mild anxiety that makes social interaction difficult, cognitive fog that impairs work performance, or emotional flatness that makes life feel gray and uninteresting. Alcohol temporarily corrects these imbalances, creating the illusion that it's improving your functioning rather than addressing deficiencies it has created.
Functioning Better Under the Influence - The Great Deception:
The question "Have you ever thought that you function better under the influence?" exposes one of alcoholism's most insidious psychological traps. This belief system develops gradually as tolerance increases and the brain adapts to alcohol's presence, creating a subjective experience where moderate intoxication feels like optimal functioning.
This perception often has some basis in reality during the middle stages of alcoholism. Because the brain has adapted to expect alcohol, small amounts can temporarily restore neurotransmitter balance, reduce anxiety, and enhance confidence. In this chemically dependent state, a person might genuinely perform better in social situations, feel more articulate in meetings, or experience enhanced creativity when moderately intoxicated.
The areas where people commonly believe they function better under the influence include social interactions, where alcohol reduces inhibition and anxiety; creative tasks, where it can temporarily lower critical thinking that might block creative flow; public speaking or performance situations, where it reduces performance anxiety; and emotional expression, where it can lower defenses that normally restrict intimate communication.
However, this enhanced functioning is illusory and temporary. What feels like improved performance is actually the temporary correction of alcohol-induced deficiencies. The brain has become so adapted to alcohol's presence that sobriety feels like impairment, and mild intoxication feels like clarity. This creates a dangerous cycle where the person begins to rely on alcohol not just for pleasure, but for what they perceive as optimal cognitive and emotional functioning.
The Progressive Nature of Balance Dependency:
The need for alcohol to achieve balance typically develops progressively, often so gradually that the person doesn't recognize what's happening. Early in this process, you might notice that you feel more confident at parties after a drink or two, or that work stress seems more manageable with a glass of wine. These observations seem reasonable and many people who don't develop alcoholism have similar experiences.
As tolerance develops, however, the baseline shifts. What once felt like normal functioning without alcohol begins to feel suboptimal. You might notice that you're more anxious in social situations when sober, less articulate in meetings without your usual lunch drink, or less able to relax in the evening without alcohol. The contrast between sober functioning and intoxicated functioning becomes more pronounced.
Eventually, sobriety begins to feel actively uncomfortable rather than simply less optimal. You might experience persistent low-level anxiety, difficulty concentrating, emotional numbness, or physical restlessness when not drinking. At this stage, alcohol isn't enhancing your functioning - it's correcting the dysfunctional state that has become your sober baseline.
The Timing Flexibility of Modern Eye Openers:
Father Martin's insight about timing reflects how alcoholism adapts to modern life and professional demands. Unlike the stereotypical skid row alcoholic who drinks openly in the morning, many people with alcoholism learn to time their eye openers around work schedules, family obligations, and social expectations.
The eye opener might be the drink you need before walking into your office building to face the day's challenges. It could be the alcohol you consume during lunch to get through afternoon meetings. It might be the immediate drink you pour when arriving home, not for celebration or relaxation, but because you feel you can't properly engage with your family until you've achieved your chemically balanced state.
Weekend eye openers often reveal the pattern most clearly because they're less constrained by work schedules. You might find that weekend mornings feel incomplete or uncomfortable until you've had your first drink, or that weekend activities require alcohol to feel enjoyable or manageable. The timing varies, but the consistent element is the sense that alcohol is necessary to achieve normal functioning.
Professional and Social Eye Openers:
The eye opener phenomenon often manifests in professional contexts in ways that can initially seem adaptive or even advantageous. You might discover that you're more confident in sales calls after a drink, more creative in brainstorming sessions with mild intoxication, or better able to handle difficult clients when you've achieved your optimal level of alcohol consumption.
These professional eye openers can be particularly dangerous because they may temporarily improve performance, creating positive reinforcement for drinking during work hours. A salesperson might close more deals, a creative professional might produce better work, or a manager might handle stress more effectively when operating at their perceived optimal level of intoxication.
Social eye openers reveal themselves in the need for alcohol before social gatherings, dates, family functions, or even casual interactions with neighbors. Without alcohol, these situations might feel awkward, anxiety-provoking, or simply less enjoyable. The eye opener isn't about getting drunk for these occasions - it's about achieving the chemical balance that makes normal social functioning feel possible and comfortable.
The Maintenance Drinking Pattern:
As the eye opener phenomenon progresses, it often evolves into a pattern of maintenance drinking - consuming alcohol throughout the day not to achieve intoxication, but to maintain the chemical balance that feels normal. This might involve having a drink before work, a drink at lunch, a drink after work, and drinks throughout the evening, with each serving to maintain rather than increase the level of alcohol in the system.
Maintenance drinking can be particularly difficult to recognize as problematic because it doesn't typically involve obvious intoxication or dramatic behavioral changes. The person might function quite well in most situations while maintaining a constant level of alcohol in their system. To outside observers, and sometimes to the person themselves, this can look like controlled, responsible drinking.
However, maintenance drinking represents a profound dependency where normal functioning has become impossible without alcohol's presence. The person has essentially created a situation where their baseline neurochemical state requires alcohol to achieve what others experience naturally. This is fundamentally different from recreational drinking or even stress-related drinking because it reflects a physiological dependency rather than a psychological preference.
The Cognitive Distortions Around Enhanced Performance:
The belief that alcohol enhances functioning creates powerful cognitive distortions that can persist even when evidence suggests otherwise. You might attribute professional successes to your optimal level of intoxication while ignoring mistakes or missed opportunities that result from alcohol use. Social interactions might feel more successful when drinking, while alcohol-related social problems are minimized or explained away.
These cognitive distortions are reinforced by the genuine relief that alcohol provides when correcting the anxiety, depression, or cognitive impairment that has become the sober baseline. Because the relief feels real and immediate, it's easy to interpret it as enhancement rather than correction of alcohol-induced dysfunction.
The distortions often extend to comparative thinking - you might believe you function better than other people when drinking, or that your drinking gives you advantages that others lack. This can create a sense of superiority or specialness around alcohol use that makes it even more difficult to recognize the underlying dependency.
Physical and Emotional Manifestations:
The need for restoration to balance manifests in both physical and emotional symptoms that alcohol temporarily alleviates. Physically, you might experience subtle tremors, restlessness, difficulty concentrating, or low-level nausea when alcohol levels drop. These symptoms might not be severe enough to recognize as withdrawal, but they create enough discomfort to make alcohol consumption feel necessary.
Emotionally, the imbalance might manifest as persistent anxiety, irritability, depression, or emotional numbness that alcohol corrects. You might feel like you can't access your full range of emotions or personality traits without alcohol's influence. Humor might feel forced, empathy might feel distant, or confidence might feel impossible to achieve without chemical assistance.
The timing of these symptoms often correlates with when alcohol typically leaves the system - you might feel increasingly uncomfortable as the day progresses if you haven't had your usual drink, or experience mounting anxiety as evening approaches and you haven't yet achieved your balanced state.
The Relationship Impact:
The eye opener phenomenon significantly affects relationships because it means that your "normal" or "best" self requires alcohol to appear. Family members might learn that certain conversations are better saved for when you've had your evening drink, or that you're more approachable and emotionally available after achieving your optimal level of intoxication.
This creates a strange dynamic where alcohol becomes necessary for intimacy and connection. Your spouse might prefer the version of you that emerges after a couple of drinks, children might find you more fun and engaging when you're moderately intoxicated, and friends might know that you're more sociable and entertaining when drinking.
However, this also means that your relationships are fundamentally dependent on a chemical substance. Without alcohol, interactions might feel stilted, emotions might seem muted, and your personality might appear constrained or anxiety-ridden. The eye opener creates a situation where genuine intimacy and connection require alcohol's mediation.
The Barrier to Recognition and Treatment:
The eye opener symptom is particularly insidious because it can masquerade as effective self-medication or performance enhancement. Unlike more obvious symptoms of alcoholism - blackouts, morning hangovers, or dramatic behavioral changes - the eye opener can appear to be solving problems rather than creating them.
This makes it difficult for both the individual and their loved ones to recognize the symptom as pathological. The person might genuinely function better in many situations when maintaining their optimal level of intoxication, and the improved functioning provides compelling evidence that their drinking is beneficial rather than harmful.
Even when problems begin to emerge, the eye opener pattern can make it difficult to connect them to alcohol use. Performance issues might be attributed to increased stress rather than alcohol dependency, relationship problems might be blamed on external factors rather than the need for chemical mediation, and physical symptoms might be explained by other health issues rather than withdrawal between drinks.
The Recovery Challenge:
Addressing the eye opener symptom in recovery presents unique challenges because it requires relearning how to function normally without alcohol's assistance. Unlike symptoms that involve obviously problematic behaviors, the eye opener represents the loss of what feels like enhanced or optimal functioning.
Recovery often involves a period where normal activities feel difficult or uncomfortable because the brain needs time to readjust its natural chemical production. Social situations might feel awkward, work performance might temporarily decline, and emotional expression might feel constrained. This can create strong temptation to return to drinking because sobriety feels like impairment rather than health.
Successful recovery from eye opener dependency often requires developing new coping strategies for anxiety, new sources of confidence for social and professional situations, and patience with the brain's gradual return to natural chemical balance. It may also require adjusting expectations and accepting that some aspects of functioning might be different in sobriety, even if they're ultimately healthier.
Father Martin's identification of the eye opener as a key symptom of alcoholism was crucial because it helped people recognize that their drinking had progressed beyond choice and into necessity. By understanding that the need for alcohol to achieve normal functioning represents a fundamental biochemical dependency rather than a personal preference or weakness, individuals could begin to address their drinking as a medical condition requiring appropriate treatment rather than a lifestyle choice requiring better willpower.
The Psychology of Secretive Consumption:
Father Martin's identification of "drinking alone to hide frequency or volume" as a cardinal symptom of alcoholism revealed one of the most psychologically complex aspects of the disease - how shame, secrecy, and isolation become both consequences of and contributors to the progression of alcohol dependency. This symptom exposes the profound shift from alcohol as a social lubricant to alcohol as a private necessity that must be hidden from others to avoid judgment and maintain the facade of control.
Drinking alone to hide frequency or volume represents a fundamental transformation in the relationship with alcohol. What begins as social drinking gradually becomes private drinking, driven by the need to consume more alcohol than would be socially acceptable or comfortable to do in front of others. This shift marks a critical point where alcohol consumption becomes incompatible with normal social interaction and requires concealment to continue.
The secrecy serves multiple psychological functions simultaneously. It protects the person from external judgment and criticism about their drinking patterns, allows for consumption at levels that would be impossible in social settings, maintains the illusion of control by keeping the true extent of drinking hidden from witnesses, and prevents interference from family members or friends who might express concern or attempt intervention.
This private drinking often becomes ritualistic and highly organized. You might develop specific routines around when, where, and how you drink alone - certain times of day when family members are absent, specific locations in the home where alcohol is consumed privately, or elaborate systems for concealing evidence of solitary drinking sessions. These rituals can become as important as the drinking itself, providing structure and predictability around alcohol consumption.
Pre-Gaming - The Strategic Preparation for Social Events:
The question "Have you ever pre-gamed a social event?" exposes a sophisticated form of drinking deception that allows for maintaining social appearances while achieving desired levels of intoxication. Pre-gaming represents strategic alcohol consumption designed to reach an optimal level of intoxication before arriving at events where drinking might be limited, monitored, or socially inappropriate.
Pre-gaming serves multiple practical purposes for someone with developing alcoholism. It ensures that you arrive at social events already at your preferred level of intoxication, reducing anxiety about whether enough alcohol will be available. It allows you to drink less visibly at the actual event while maintaining your desired level of impairment. It provides a buffer against social situations that might be uncomfortable or anxiety-provoking without adequate alcohol preparation.
The pre-gaming pattern often develops gradually and can initially seem like reasonable behavior. You might start by having a drink at home before going to restaurants where alcohol is expensive, or having a couple of drinks before parties where you're not sure about the alcohol situation. However, as tolerance increases and dependency develops, pre-gaming becomes less about practical considerations and more about ensuring adequate alcohol levels for basic social functioning.
Advanced pre-gaming can involve complex calculations about timing, absorption rates, and social expectations. You might drink specific amounts at specific times to achieve peak intoxication exactly when you arrive at events. You might coordinate pre-gaming with eating patterns to control absorption rates, or plan bathroom breaks during events to supplement your pre-gaming with additional alcohol consumption.
The sophistication of pre-gaming strategies often reflects the level of planning and priority that alcohol has assumed in your life. What appears to others as spontaneous social drinking is actually the result of careful preparation and strategic consumption designed to maintain optimal intoxication levels throughout social interactions.
The Preference for Non-Sharing - Protecting Personal Supply:
The reluctance to share alcohol reveals how scarcity thinking develops around alcohol consumption. When drinking progresses to dependency, alcohol becomes too valuable and necessary to share freely with others. What once might have been generous sharing of drinks becomes careful hoarding and protection of personal alcohol supplies.
This preference for not sharing manifests in various ways that can be subtle or obvious depending on the social context. You might buy specific amounts of alcohol calculated for personal consumption only, becoming anxious when others help themselves to "your" drinks. You might make excuses to avoid situations where sharing is expected, or you might share grudgingly while mentally calculating how the sharing affects your own alcohol availability.
The non-sharing preference often extends to specific types or qualities of alcohol. You might keep expensive or preferred alcohol hidden while offering guests cheaper alternatives, or you might have designated "personal" alcohol that others are not supposed to touch. This creates a two-tier system where some alcohol is for social consumption and other alcohol is reserved for private use.
In family settings, the preference for non-sharing can create tension and confusion. Family members might notice that certain bottles or types of alcohol are off-limits, or that there are unspoken rules about what alcohol can be consumed by whom. This can lead to conflict and resentment as family members feel unwelcome to partake in alcohol that is ostensibly for household use.
The underlying psychology of non-sharing reflects the transition from viewing alcohol as a social enhancer to viewing it as a personal necessity. When alcohol becomes necessary for emotional regulation, anxiety management, or basic functioning, sharing it with others feels like giving away medicine rather than offering hospitality.
The Burden of Shame and Guilt - Feeling Judged by Usage:
The shame and guilt associated with alcohol consumption create a powerful feedback loop that drives both continued drinking and increased secrecy. The awareness that your drinking patterns are abnormal or excessive generates shame, which then drives the need to hide the drinking, which in turn increases the sense of shame about the deception and secrecy.
This shame often has multiple layers and sources. There's shame about the quantity of alcohol consumed, shame about drinking alone, shame about the priority that alcohol has assumed in your life, shame about the deception and lying that concealment requires, and shame about being unable to control or moderate your consumption despite repeated attempts.
The feeling of being judged, whether real or perceived, becomes a constant presence that influences decisions about when, where, and how to drink. You might avoid certain social situations where your drinking would be scrutinized, decline invitations where alcohol consumption might be limited or monitored, or feel constantly defensive about your drinking habits even when no one is actually questioning them.
This perceived judgment often leads to elaborate justification systems and defensive strategies. You might prepare explanations for your drinking patterns before anyone asks, become hypervigilant about how much others are drinking to ensure you're not obviously consuming more, or develop strategies for appearing less intoxicated than you actually are to avoid drawing attention to your alcohol consumption.
The shame spiral often becomes self-perpetuating: shame about drinking leads to secretive drinking, which increases shame about deception, which leads to more isolation and drinking, which generates more shame. This cycle can become increasingly difficult to break without external intervention because the very act of hiding the problem prevents getting help for it.
The Evolution of Solitary Drinking Patterns:
Drinking alone typically evolves through predictable stages that reflect the increasing priority of alcohol in your life. Early solitary drinking might involve having a drink while cooking dinner or unwinding after work when other family members aren't around. This can seem normal and healthy - many people enjoy a glass of wine while preparing dinner or a beer while doing yard work.
As dependency develops, solitary drinking becomes more intentional and necessary. You might begin to create opportunities to drink alone by volunteering for errands that allow you to stop for drinks, staying up after family members go to bed to continue drinking, or waking up early to drink before others are awake. The drinking becomes less incidental and more purposeful.
Advanced solitary drinking often involves elaborate planning and concealment strategies. You might have multiple hiding places for alcohol throughout your home, car, or workplace. You might develop complex systems for disposing of evidence - empty bottles, cans, or glasses that would reveal the extent of your consumption. You might coordinate your drinking with family schedules to ensure privacy during consumption.
The most advanced forms of solitary drinking can involve creating entirely separate drinking lives that family and friends know nothing about. This might include stopping at bars during commutes, drinking in cars or other private locations, or maintaining alcohol supplies at work or other locations where you can drink without detection. At this stage, the effort required to maintain secrecy can become almost as consuming as the drinking itself.
The Social Isolation Progression:
The need to hide drinking frequency and volume often leads to increasing social isolation as maintaining the deception becomes more difficult in group settings. Social events become stressful because they require careful management of alcohol consumption to avoid revealing the true extent of your drinking patterns.
You might begin declining social invitations where your drinking would be noticeable or limited, avoiding situations where others might comment on your alcohol consumption, or feeling anxious at events where you can't control the availability or quantity of alcohol. This can lead to a gradual withdrawal from social activities and relationships.
The isolation often becomes a vicious cycle: drinking alone becomes more comfortable and predictable than managing social drinking situations, but the isolation increases depression and anxiety, which then drives more drinking. Social skills may deteriorate from lack of practice interacting sober, making social situations even more anxiety-provoking and requiring more alcohol to manage.
Family relationships often suffer as the need for private drinking time takes priority over family activities. You might become resentful of family obligations that interfere with drinking, or family members might notice your withdrawal and emotional unavailability when you haven't been able to drink privately.
The Workplace Dimension:
Hiding drinking frequency and volume can extend into professional environments, creating additional layers of complexity and risk. You might drink during lunch breaks, keep alcohol in your office or car for consumption during the workday, or time your drinking around work schedules to ensure you're never completely sober during work hours.
Professional hiding strategies can be particularly sophisticated because the stakes are high - losing employment due to alcohol-related issues can have devastating consequences. You might use mouthwash, perfume, or eye drops to mask evidence of drinking, time your consumption to minimize obvious impairment during important meetings, or develop elaborate explanations for any alcohol-related performance issues.
The stress of maintaining professional appearances while managing alcohol dependency can become overwhelming. The fear of discovery at work can drive even more secretive drinking patterns, as you try to balance the need for alcohol with the requirements of professional functioning.
The Technology and Modern Concealment:
Modern technology has created new opportunities and challenges for hiding drinking patterns. Smartphones can be used to coordinate alcohol purchases, find drinking locations, or communicate with others about drinking without family members' knowledge. However, technology also creates digital trails that can reveal drinking patterns - credit card statements, location tracking, or social media posts that contradict claims about drinking behavior.
Online alcohol delivery services can facilitate secretive drinking by allowing alcohol purchases without leaving home or encountering familiar people at liquor stores. However, these services also create records and delivery evidence that must be managed to maintain secrecy.
Social media presents particular challenges because alcohol-related posts or photos can contradict attempts to minimize drinking to family and friends. You might find yourself carefully managing your online presence to avoid revealing the extent of your alcohol consumption or the frequency of your drinking occasions.
The Financial Concealment Component:
Hiding drinking frequency and volume often requires concealing the financial cost of alcohol consumption. As tolerance increases and consumption grows, alcohol expenses can become significant and difficult to explain within household budgets. This can lead to elaborate financial deception strategies.
You might use cash for alcohol purchases to avoid credit card records, maintain separate accounts for alcohol-related expenses, or create false explanations for alcohol-related charges on family accounts. Some people develop complex systems for hiding alcohol costs within other expense categories - claiming alcohol purchases were for groceries, entertainment, or business expenses.
The financial stress of maintaining high levels of alcohol consumption while hiding the costs can create additional pressure that drives more drinking. You might find yourself choosing between necessary expenses and alcohol, or going into debt to maintain your drinking patterns while keeping the financial impact hidden from family members.
The Impact on Intimate Relationships:
The need to hide drinking creates profound barriers to intimacy in close relationships. Partners may sense that something is being hidden without understanding what it is, creating tension and distance in the relationship. The energy required to maintain deception can leave little emotional availability for genuine connection and intimacy.
Sexual relationships can be particularly affected because alcohol consumption often peaks during evening hours when physical intimacy typically occurs. Partners might notice patterns of unavailability, emotional distance, or physical symptoms that they can't fully understand or address because the underlying alcohol consumption is hidden.
The deception required to hide drinking can fundamentally alter the character of relationships, introducing elements of dishonesty and manipulation that contaminate other aspects of the relationship. Even when partners suspect alcohol-related issues, the secretive nature of the drinking makes it difficult to address problems directly or seek appropriate help.
The Physical Health Concealment:
Hiding drinking frequency and volume often involves concealing alcohol-related health symptoms from healthcare providers, family members, and even from yourself. You might minimize alcohol consumption when completing medical history forms, avoid medical appointments when alcohol-related symptoms are obvious, or attribute alcohol-related health issues to other causes.
This health concealment can have serious medical consequences because healthcare providers cannot properly assess or treat conditions when they don't have accurate information about alcohol consumption. Alcohol interactions with medications, alcohol-related organ damage, or alcohol withdrawal symptoms might go unrecognized and untreated because of deliberate concealment of drinking patterns.
The physical evidence of heavy drinking - changes in appearance, sleep patterns, energy levels, or cognitive functioning - often requires additional concealment strategies. You might use makeup to hide facial changes, caffeine or other substances to mask fatigue, or develop explanations for physical symptoms that don't involve alcohol.
Breaking Through the Secrecy Barrier:
Father Martin's identification of this symptom was crucial because it helped people recognize that the need for secrecy around drinking was itself a symptom of alcoholism rather than simply a reasonable response to social expectations. The shame and secrecy that drive hidden drinking also prevent seeking help, creating a self-perpetuating cycle that can only be broken by acknowledging the problem and reaching out for support.
Recovery often requires dismantling the elaborate systems of concealment and deception that have been built around drinking. This can be terrifying because it involves revealing to others the true extent of alcohol consumption and the sophisticated efforts that have been made to hide it. However, this revelation is often necessary for accessing appropriate treatment and rebuilding honest relationships.
The process of becoming honest about drinking patterns often reveals how much energy and mental resources have been devoted to concealment. People in recovery frequently describe feeling exhausted by the constant vigilance required to hide their drinking and relieved to no longer need to maintain these elaborate deception systems.
Father Martin's insight into secretive drinking patterns helped people understand that their elaborate concealment strategies were symptoms of a disease rather than moral failings or character defects. By recognizing the shame-secrecy-isolation cycle as part of alcoholism's progression, individuals could begin to address the underlying dependency rather than simply trying harder to hide it more effectively.
The Psychology of Pattern Manipulation:
Father Martin's identification of "changing the patterns" as a symptom of alcoholism revealed one of the most sophisticated and psychologically revealing aspects of the disease - the elaborate attempts to regain control over alcohol consumption through manipulation of external variables while avoiding the fundamental issue of dependency itself. This symptom demonstrates how the addicted mind seeks to solve the problem of alcoholism through everything except stopping drinking entirely.
The tendency to change drinking patterns represents a complex psychological defense mechanism that allows continued alcohol consumption while maintaining the illusion of control and progress. Father Martin understood that these pattern changes reflect the internal awareness that drinking has become problematic, combined with the desperate desire to continue drinking without the negative consequences.
This symptom reveals the sophisticated reasoning capabilities of the addicted mind - the ability to analyze drinking patterns, identify potential problems, and develop elaborate solutions that address everything except the core issue of alcohol dependency. The pattern changes create the appearance of taking constructive action while actually avoiding the most effective solution: abstinence.
Each pattern change typically follows the same psychological sequence: recognition that current drinking patterns are creating problems, analysis of what specific aspects of the current pattern might be causing issues, development of a new pattern designed to eliminate those specific problems, implementation of the new pattern with initial optimism and control, gradual return of problems as the underlying dependency reasserts itself, and eventual recognition that the new pattern has also become problematic, leading to the next round of changes.
Switching Brands - The Illusion of Substance Control:
Brand switching represents one of the most common and psychologically revealing pattern changes in alcoholism. The logic appears sound: if drinking Brand X is causing problems, switching to Brand Y might solve those problems while allowing continued alcohol consumption. This approach treats alcoholism as if it were an allergy or sensitivity to specific alcohol types rather than a dependency on the psychoactive effects of ethanol itself.
The brand switching often follows predictable pathways based on perceived differences in alcohol types. You might switch from hard liquor to wine, believing that wine is more civilized and less likely to cause problems. The switch might involve moving from high-alcohol content beverages to lower-alcohol alternatives, based on the theory that the alcohol concentration rather than the consumption pattern is the issue.
Geographic or cultural associations often influence brand switching decisions. Switching from domestic to imported alcohol might feel like upgrading to more sophisticated drinking habits. Moving from cheap alcohol to expensive brands can create the illusion that quality rather than quantity is the important factor. Some people switch to brands associated with health consciousness - organic wines, craft beers, or "natural" spirits - as if the processing methods rather than the alcohol content were the problem.
The brand switching can become increasingly elaborate and specific. You might avoid certain types of alcohol during weekdays but allow them on weekends, switch between different alcohol types based on social situations, or develop complex rules about which brands are acceptable in which circumstances. Some people create hierarchies of alcohol acceptability, with some brands designated as "safe" and others as "dangerous."
The psychological relief provided by brand switching can be profound but temporary. The new brand initially feels like a fresh start and evidence of control and good judgment. However, as tolerance develops and consumption increases with the new brand, the same problems eventually emerge. The disappointment and confusion when brand switching fails to solve drinking problems often leads to more extreme pattern changes or, ironically, a return to previous brands with the rationalization that "at least I know how those affect me."
Switching Substances - The Cross-Addiction Shuffle:
Substance switching represents a more dramatic form of pattern manipulation that often reflects the recognition that alcohol specifically has become problematic. However, rather than addressing the underlying addictive tendencies, substance switching attempts to find alternative intoxicants that might provide similar effects without the negative consequences associated with alcohol.
Common substance switches include moving from alcohol to marijuana, believing that cannabis is less harmful or addictive. Some people switch to prescription medications - anxiety medications, sleep aids, or pain relievers - that can provide relaxation or euphoria similar to alcohol's effects. Others might switch to over-the-counter substances like cough medicines or sleep aids that contain psychoactive ingredients.
The rationale for substance switching often involves comparing the perceived risks and benefits of different intoxicants. Marijuana might seem safer because it's becoming legal in many places and is often portrayed as natural and harmless. Prescription medications might feel safer because they're prescribed by doctors and regulated by the FDA. Some people switch to substances that seem more socially acceptable or professional - using anxiety medications instead of alcohol for workplace stress management.
However, substance switching rarely addresses the underlying psychological and neurological factors that drive addictive behavior. The same patterns of tolerance, dependency, and loss of control often emerge with the new substance. Additionally, substance switching can create new categories of problems - legal issues with illegal drugs, health complications from prescription drug misuse, or interactions between different substances.
Some people develop rotation systems between multiple substances, believing that avoiding dependency on any single substance will prevent addiction. This might involve alternating between alcohol and marijuana, cycling through different prescription medications, or using alcohol some days and other substances on other days. These rotation systems can create the illusion of control while actually representing multiple concurrent dependencies.
Designated Days - Temporal Control Strategies:
The implementation of designated drinking days represents one of the most psychologically sophisticated attempts to control alcoholism through external structure. This approach acknowledges that daily drinking has become problematic while attempting to maintain alcohol consumption within artificially imposed temporal boundaries.
Common designated day systems include restricting drinking to weekends only, limiting alcohol to specific days of the week, implementing "dry days" alternated with "drinking days," or creating seasonal restrictions where alcohol is only consumed during certain times of year. Some people create elaborate calendar systems with drinking days marked in advance, believing that pre-planning will create accountability and control.
The psychology behind designated days often involves the belief that the timing of alcohol consumption, rather than the consumption itself, is the primary problem. The logic suggests that if drinking can be confined to specific times, it won't interfere with work, family responsibilities, or health goals. This approach treats alcoholism as if it were a scheduling problem rather than a medical condition.
Weekend-only drinking is perhaps the most common designated day strategy. The rationale appears sound: avoiding alcohol during work days prevents professional problems while allowing relaxation and socialization during weekends. However, as tolerance develops, weekend consumption often escalates dramatically to compensate for weekday abstinence. What begins as moderate weekend drinking can evolve into intense binge drinking sessions that create their own set of problems.
The designated day approach often leads to anticipatory behavior that undermines its effectiveness. You might find yourself watching the clock on Thursday evening, eagerly awaiting Friday's designated drinking time. Work performance might suffer on Fridays due to anticipation of evening drinking, or on Mondays due to weekend alcohol recovery. The restriction can create an obsessive focus on alcohol that paradoxically increases its importance rather than decreasing it.
Many people experience "day creep" where designated drinking days gradually expand. Wednesday might be added because it's "almost the weekend." Sunday drinking might extend into Monday because it's still "part of the weekend." Special occasions, holidays, or stressful events might justify exceptions to the designated day rules. Eventually, the designated day system often collapses entirely, but not before creating the illusion of control for extended periods.
Switching Suppliers - Geographic and Social Control:
Supplier switching represents an attempt to control alcoholism through manipulation of purchasing patterns and social environments. This strategy often reflects shame about alcohol consumption levels and attempts to avoid judgment from store clerks, bartenders, or other people who might notice excessive purchasing patterns.
The supplier switching can involve rotating between different liquor stores to avoid appearing as a regular customer at any single location. You might drive to stores in different neighborhoods, shop at different times of day to encounter different staff members, or alternate between chain stores and independent retailers. Some people develop elaborate geographical patterns for alcohol purchases, ensuring that no single supplier sees the full extent of their consumption.
Online alcohol delivery services have created new opportunities for supplier switching and consumption concealment. You might rotate between different delivery services, use different payment methods to spread purchases across multiple accounts, or coordinate deliveries with family schedules to avoid detection. The convenience and anonymity of online purchasing can actually facilitate increased consumption while creating the illusion of discretion.
Bar and restaurant supplier switching follows similar patterns. You might rotate between different establishments to avoid becoming known as a heavy drinker at any single location. This can involve developing complex social calendars designed to distribute alcohol consumption across multiple venues, creating the appearance of social drinking while actually facilitating solitary consumption in public settings.
The psychology of supplier switching often involves projection of judgment onto others. You might believe that store clerks are monitoring your purchases, that bartenders are judging your consumption, or that restaurant servers are keeping track of how much you drink. Whether or not this judgment actually exists, the perceived scrutiny drives the need to distribute consumption across multiple suppliers to avoid detection.
Supplier switching can also involve attempts to access different types or qualities of alcohol. You might shop at upscale stores for "special occasion" alcohol while purchasing daily consumption alcohol at discount retailers. This creates artificial categories of drinking that can help rationalize consumption levels - the expensive alcohol feels like legitimate social drinking while the cheap alcohol doesn't "count" as much.
Buying Smaller Amounts More Frequently - Quantity Control Illusions:
The strategy of purchasing smaller quantities more frequently represents one of the most psychologically complex pattern changes because it attempts to address consumption concerns while actually facilitating increased access to alcohol. This approach reflects the recognition that large alcohol purchases are problematic while missing the fact that frequent small purchases can result in even higher overall consumption.
The logic behind smaller, frequent purchases often involves avoiding the embarrassment or concern associated with buying large quantities of alcohol at one time. A bottle of wine with dinner ingredients seems more acceptable than a case of wine. A single bottle of whiskey appears more reasonable than multiple bottles, even if the single bottle is replaced every few days rather than lasting weeks or months.
This purchasing pattern can actually increase consumption because it ensures a constant fresh supply of alcohol and eliminates the natural brake that running out of alcohol provides. When alcohol supplies are limited to what's currently in the house, consumption might naturally moderate when supplies run low. However, frequent purchasing ensures that running out never becomes a limiting factor.
The frequent purchasing often involves developing elaborate justification systems for each purchase. Every trip to the store has a legitimate primary purpose - groceries, household items, or work supplies - with alcohol added as a seemingly incidental additional item. This creates the illusion that alcohol purchasing is spontaneous and occasional rather than planned and systematic.
Some people develop rotation systems for purchase timing and locations that create the appearance of infrequent purchasing while actually maintaining constant supply. You might buy alcohol every few days but at different stores, creating the impression to each store clerk that you only purchase alcohol occasionally. The mental energy required to coordinate these purchasing patterns can become significant, reflecting how much priority alcohol has assumed in daily planning.
The smaller quantity purchases often involve price comparisons and efficiency calculations that reveal the sophisticated planning involved in maintaining alcohol supplies. You might calculate the cost per unit of different bottle sizes, plan purchasing routes to minimize travel time and cost, or coordinate alcohol purchases with other errands to maximize efficiency.
The Escalation of Pattern Changes:
Father Martin observed that pattern changes typically become more frequent and elaborate as alcoholism progresses. Early pattern changes might be simple and occasional - switching from beer to wine for a few weeks, or avoiding alcohol on Sundays. As the disease progresses, pattern changes become more complex, frequent, and desperate.
Advanced pattern manipulation can involve multiple simultaneous strategies: switching brands weekly, implementing complex calendar systems for consumption timing, rotating between multiple suppliers, alternating between different substances, and constantly adjusting quantity and frequency parameters. The mental energy required to maintain these elaborate systems can become exhausting, yet the complexity creates the illusion of control and scientific approach to drinking management.
The pattern changes often follow cycles of increasing restriction followed by rebellion and relaxation of rules. A period of strict weekend-only drinking might be followed by a "special occasion" exception that opens the door to more frequent consumption. Brand restrictions might be abandoned during stressful periods with promises to return to the "safe" brands later.
The Underlying Psychological Functions:
Father Martin understood that pattern changes serve crucial psychological functions that extend beyond the practical goal of controlling alcohol consumption. These changes provide evidence to yourself and others that you're aware of potential problems and taking constructive action to address them. They create the illusion of progress and control without requiring the sacrifice of alcohol consumption itself.
Pattern changes also serve as delay tactics that postpone the need to confront the fundamental issue of alcohol dependency. Each new pattern provides hope that this approach will finally solve the problem, buying time and justification for continued drinking. The pattern change process can continue for years, providing a series of experiments that feel scientific and rational while avoiding the obvious solution.
The changes often reflect genuine attempts to harm reduction, demonstrating that the person recognizes problems and wants to improve their situation. However, the focus on external manipulation rather than internal change reveals the persistent denial about the nature of alcoholism as a progressive disease that requires comprehensive treatment rather than pattern modification.
The Social and Family Impact:
Pattern changes often confuse and frustrate family members and friends who observe the elaborate efforts to control drinking while missing the obvious solution of stopping entirely. Loved ones might initially feel hopeful when pattern changes are announced, interpreting them as evidence of progress and commitment to change.
However, as pattern changes repeatedly fail to solve the underlying problems, family members often become skeptical of new schemes and promises. The cycle of pattern change, temporary improvement, gradual deterioration, and new pattern change can create a sense of futility and exhaustion among those who care about the person with alcoholism.
Children in families affected by alcoholism often become confused by the constantly changing rules and restrictions around alcohol. They might learn that certain brands, days, or quantities are "good" while others are "bad," without understanding the underlying logic or the fact that the rules themselves are symptoms of a larger problem.
The Barrier to Treatment:
The pattern change symptom represents one of the most significant barriers to seeking appropriate treatment for alcoholism because it provides the illusion that the problem can be solved through self-management and willpower. Each pattern change feels like a reasonable experiment in moderation management, delaying recognition that controlled drinking is impossible for people with alcoholism.
The sophisticated reasoning involved in pattern development can actually reinforce denial about the severity of the drinking problem. The ability to analyze drinking patterns, develop complex strategies, and implement systematic changes can feel like evidence of control and rationality rather than symptoms of advanced alcoholism.
Treatment often requires helping people recognize that the energy and creativity they've devoted to pattern manipulation demonstrates both the severity of their alcohol dependency and their capacity for the systematic thinking required for recovery. The same analytical skills used for pattern development can be redirected toward recovery planning and relapse prevention.
Father Martin's identification of pattern changing as a symptom rather than a solution was revolutionary because it helped people understand that their elaborate attempts at control were actually evidence of loss of control. By recognizing pattern manipulation as part of the disease rather than evidence of recovery progress, individuals could begin to consider more fundamental approaches to addressing their relationship with alcohol, ultimately leading to the recognition that complete abstinence might be the only effective pattern change for someone with alcoholism.
The Progressive Nature of Social Isolation:
Father Martin's identification of "anti-social behavior" as a cardinal symptom of alcoholism revealed one of the most devastating and progressive aspects of the disease - how alcohol dependency systematically dismantles social connections, relationships, and community ties that are essential for human wellbeing and recovery. This symptom exposes how alcoholism transforms from a social activity into an isolating force that ultimately dictates and destroys the very relationships that might otherwise provide support and intervention.
The anti-social behavior associated with alcoholism doesn't typically begin as deliberate isolation or misanthropy. Instead, it develops gradually as alcohol consumption patterns become increasingly incompatible with normal social functioning. Father Martin understood that this isolation often begins subtly, with small adjustments to social patterns that seem reasonable and temporary but eventually compound into profound disconnection from others.
Early isolation might manifest as declining invitations where alcohol won't be available or will be limited. You might start avoiding dinner parties where wine service is controlled by hosts, work events where drinking is monitored or inappropriate, or family gatherings where your consumption might be scrutinized by relatives who know your drinking history. These initial avoidances seem practical and manageable - simply choosing social environments that are more compatible with your drinking preferences.
As tolerance develops and consumption increases, the criteria for acceptable social situations become increasingly narrow. You might find yourself only comfortable in environments where heavy drinking is normalized or expected - certain bars, drinking-focused social groups, or events specifically organized around alcohol consumption. Social activities that don't center on drinking begin to feel pointless, uncomfortable, or anxiety-provoking.
The progression often involves a gradual shift from avoiding specific social situations to avoiding social interaction entirely. Phone calls go unanswered, invitations are declined with increasingly elaborate excuses, and spontaneous social contact is discouraged. The effort required to maintain social facades while hiding drinking patterns becomes exhausting, making isolation feel like the easier and safer option.
The Addiction Dictating Geographic and Social Choices:
Father Martin's insight that "the addiction dictates the places we go and who we go there with" reveals how alcoholism fundamentally reorganizes life priorities and decision-making processes. Rather than social choices being made based on personal interests, relationship value, or life goals, they become subordinated to alcohol access and consumption requirements.
Geographic choices increasingly revolve around alcohol availability and consumption opportunities. You might choose restaurants based on their alcohol selection rather than food quality, select hotels during travel based on proximity to bars or in-room alcohol policies, or plan vacation destinations around drinking opportunities rather than personal interests or family preferences. The location of your home might be influenced by proximity to liquor stores, bars, or other alcohol sources.
Daily routines become organized around alcohol access and consumption timing. Grocery store routes are planned to include liquor store stops, work schedules are preferred if they allow for earlier drinking times, and social commitments are arranged around alcohol availability. Even mundane decisions like which gas station to use might be influenced by whether they sell alcohol and whether purchasing there fits into your consumption concealment strategies.
The people you choose to spend time with increasingly become filtered through their relationship to your drinking. Friends who don't drink heavily might be gradually phased out because their presence makes your consumption feel conspicuous or inappropriate. Social groups that focus on activities incompatible with drinking - fitness groups, religious organizations, or professional development activities - become sources of anxiety rather than enjoyment.
Conversely, relationships with other heavy drinkers might be prioritized not because of genuine friendship or compatibility, but because they provide cover for your own consumption and eliminate the need to explain or justify drinking patterns. These relationships often become superficial and transactional, revolving around shared drinking rather than genuine personal connection.
The Mechanics of Avoidance:
The avoidance patterns in alcoholism are often highly sophisticated and can appear reasonable to outside observers, making them difficult to identify as symptoms of a progressive disease. The avoidance typically begins with situations that genuinely interfere with drinking patterns but gradually expands to include any social interaction that might reveal the extent of alcohol dependency or interfere with consumption routines.
Work-related social avoidance often begins with declining after-work events where drinking might be inappropriate or limited. Office parties where alcohol service is controlled, business dinners where professional behavior is expected, or networking events where sobriety is important for making good impressions become sources of anxiety rather than opportunities. The fear of being unable to drink adequately or of drinking too much in professional settings drives avoidance of career development opportunities.
Family event avoidance frequently follows patterns related to the likelihood of drinking scrutiny or interference. You might avoid family gatherings where relatives have previously expressed concern about your drinking, events where children are present and adult behavior is more closely monitored, or celebrations where your drinking patterns might be compared to those of other family members. Holiday gatherings become particularly problematic because they often involve extended time periods where drinking patterns are visible to others.
Religious or spiritual community avoidance often reflects the conflict between alcohol dependency and value systems that discourage excessive drinking. Church services, religious social events, or spiritual retreat activities become uncomfortable because they highlight the contradiction between stated values and actual behavior. The judgment, whether real or perceived, from religious communities can drive progressive withdrawal from spiritual practices and support systems.
Health-related activity avoidance becomes common as alcohol consumption increases and physical fitness deteriorates. Gym memberships might be abandoned, sporting activities might be declined, and medical appointments might be postponed to avoid discussions about alcohol consumption or alcohol-related health symptoms. The avoidance extends to any activity that might reveal the physical or cognitive impact of heavy drinking.
The Psychology of Disconnection:
The disconnection associated with alcoholism operates on multiple levels simultaneously - emotional, physical, intellectual, and spiritual. Father Martin recognized that alcohol creates a barrier between the individual and authentic relationship with others, even when social interaction continues. The person may be physically present in social situations but emotionally and intellectually unavailable due to alcohol's effects on cognitive and emotional functioning.
Emotional disconnection often manifests as the inability to engage genuinely with others' feelings, experiences, or needs. Alcohol's effects on emotional regulation and empathy can make it difficult to respond appropriately to others' joys, sorrows, or concerns. Conversations become superficial because deeper emotional engagement requires cognitive and emotional resources that are impaired by alcohol consumption or compromised by preoccupation with drinking.
Intellectual disconnection occurs when alcohol's cognitive effects interfere with the ability to engage in meaningful conversation, problem-solving, or shared intellectual activities. You might find yourself unable to follow complex discussions, contribute meaningfully to group decisions, or engage with ideas that require sustained concentration. This intellectual impairment can lead to feelings of inadequacy and further social withdrawal.
Spiritual disconnection often involves the loss of connection to meaning, purpose, and values that transcend immediate personal gratification. Alcohol can interfere with the ability to engage with larger questions of meaning, moral development, or spiritual growth. Religious or philosophical discussions might feel threatening because they highlight the contradiction between alcohol-centered living and deeper value systems.
The disconnection often becomes self-perpetuating as alcohol increasingly becomes the primary relationship in your life. Human relationships require emotional availability, reliability, and genuine interest in others' wellbeing - qualities that become difficult to maintain when alcohol consumption becomes the organizing principle of daily life. As relationships deteriorate due to alcohol-related unavailability, the resulting loneliness and social pain often drive increased drinking, creating a vicious cycle.
The Impact on Intimate Relationships:
Anti-social behavior in alcoholism particularly devastates intimate relationships because these connections require the highest levels of emotional availability, honesty, and vulnerability. Alcohol dependency creates barriers to genuine intimacy that can persist even during periods of sobriety because the habits of emotional unavailability and defensive behavior become deeply ingrained.
Romantic relationships suffer as alcohol consumption takes priority over partner needs and relationship maintenance. Date nights become opportunities for drinking rather than connection, conflicts are avoided or mishandled due to alcohol's emotional effects, and physical intimacy may be impaired by alcohol's physiological impacts. Partners often report feeling like they're in a relationship with alcohol rather than with the person, as drinking patterns dictate mood, availability, and behavior.
Parental relationships become particularly tragic as alcohol dependency interferes with the emotional presence and consistency that children need for healthy development. Parent-child activities might be declined if they interfere with drinking routines, emotional support might be unavailable during times of high alcohol consumption, and children may learn to avoid approaching parents during drinking periods. The unpredictability of alcohol-affected mood and behavior can create anxiety and insecurity in children.
Family relationships often deteriorate as alcohol consumption creates increasing conflict, disappointment, and tension. Family members may feel helpless watching someone they love become progressively more isolated and unavailable. The person with alcoholism might perceive family concern as judgment or interference, leading to defensive withdrawal from family contact.
The Professional and Career Consequences:
Anti-social behavior in alcoholism often extends into professional environments, creating career limitations and workplace isolation that can have lasting economic and professional consequences. The avoidance patterns that develop around alcohol dependency can interfere with networking, career development, and professional relationship building that are essential for advancement in most fields.
Professional networking events become problematic because they often involve controlled alcohol service or occur during times when you prefer to be drinking privately. Industry conferences, professional development workshops, or continuing education opportunities might be avoided if they interfere with drinking routines or create anxiety about alcohol availability. These avoidances can limit career growth and professional development over time.
Workplace socializing often becomes strained as alcohol dependency creates barriers to authentic colleague relationships. Lunch meetings where alcohol isn't served, after-work team building activities that don't focus on drinking, or office social events where consumption is monitored become sources of anxiety rather than relationship building opportunities. Colleagues may notice the pattern of avoidance and begin to perceive the person as antisocial or uninterested in team participation.
Mentorship relationships, both as mentor and mentee, often suffer as alcohol dependency interferes with the emotional availability and reliability required for effective professional guidance. The inability to engage genuinely with others' professional development needs or to be consistently available for guidance can damage professional reputation and limit career advancement opportunities.
The Community and Social Institution Withdrawal:
The anti-social behavior associated with alcoholism often involves progressive withdrawal from community institutions and social organizations that provide meaning, purpose, and social support. These withdrawals represent significant losses of social capital and support systems that are crucial for both general wellbeing and potential recovery.
Religious community withdrawal often occurs as alcohol dependency creates conflict with spiritual values and community expectations around behavior and lifestyle. The judgment, whether real or perceived, from religious communities can drive progressive disengagement from worship services, religious education, volunteer activities, and social events. This withdrawal eliminates important sources of meaning, purpose, and social support.
Civic and community organization participation often declines as alcohol consumption takes priority over community involvement. Volunteer activities, neighborhood associations, professional organizations, or charitable work might be abandoned if they interfere with drinking routines or create anxiety about alcohol availability. These withdrawals reduce social connection and eliminate opportunities for meaningful contribution to community wellbeing.
Educational and learning community withdrawal can occur as alcohol affects cognitive functioning and interferes with the ability to engage in sustained learning activities. Adult education classes, book clubs, discussion groups, or skill development workshops might be avoided if they require sobriety, sustained concentration, or regular attendance that conflicts with drinking patterns.
The Creation of Alcohol-Centered Social Networks:
As authentic social connections deteriorate, alcoholism often drives the creation of new social networks that revolve around drinking activities and accommodate heavy alcohol consumption. However, these relationships are typically superficial and transactional, lacking the depth and reciprocity of genuine friendship.
Bar relationships often become primary social connections, but they're typically based on shared drinking rather than genuine personal compatibility or mutual support. These relationships rarely extend beyond drinking contexts and may not survive attempts to reduce or eliminate alcohol consumption. The apparent social connection masks underlying isolation because the relationships depend on continued alcohol use.
Drinking buddy relationships can provide the illusion of social connection while actually enabling continued isolation from authentic relationships. These connections often involve mutual enablement where each person's drinking problem is normalized by the other's similar patterns. The relationships may feel supportive but actually prevent recognition of alcohol-related problems and interfere with motivation for change.
Online communities focused on drinking can provide social connection while enabling continued isolation from real-world relationships. Social media groups, forums, or apps that celebrate drinking culture can create a sense of belonging while actually supporting continued alcohol dependency and discouraging real-world social engagement.
The Vicious Cycle of Isolation and Drinking:
Father Martin understood that anti-social behavior in alcoholism creates a self-perpetuating cycle where isolation drives increased drinking, which in turn drives further isolation. This cycle becomes increasingly difficult to break without external intervention because the very isolation that results from alcohol dependency eliminates access to the social support systems that might otherwise motivate and support change.
The loneliness resulting from social isolation becomes a powerful trigger for increased alcohol consumption. Drinking provides temporary relief from the pain of disconnection while simultaneously preventing the authentic social engagement necessary to rebuild genuine relationships. The short-term relief reinforces the use of alcohol as a solution to social pain while actually perpetuating the underlying problem.
Social anxiety, often exacerbated by alcohol withdrawal symptoms, makes social engagement increasingly difficult without alcohol's temporary anxiety relief. This creates a dependency on alcohol for any social interaction, which then interferes with the development of genuine social skills and confidence. The cycle reinforces itself as social situations become impossible to navigate without alcohol, leading to further isolation and increased drinking.
The Impact on Personal Identity and Self-Worth:
The progressive social isolation associated with alcoholism often profoundly affects personal identity and self-worth as social roles and relationships that previously provided meaning and validation are lost or damaged. The person may begin to see themselves as fundamentally antisocial, unlikeable, or incapable of maintaining relationships, which can drive further withdrawal and increased alcohol consumption.
Professional identity often suffers as career advancement stagnates due to social avoidance and alcohol-related performance issues. The loss of professional achievements and recognition can undermine self-worth and create additional motivation for alcohol use as a coping mechanism. The downward spiral of professional isolation and declining performance reinforces negative self-perception.
Family and parental identity can be devastated as alcohol dependency interferes with the ability to fulfill family roles and responsibilities. The guilt and shame associated with alcohol-related neglect or unavailability can drive further isolation and drinking, creating additional distance from family relationships that might otherwise provide motivation for change.
Breaking the Cycle of Anti-Social Behavior:
Recovery from alcoholism typically requires consciously addressing the anti-social behavior patterns that have developed alongside alcohol dependency. This often involves gradually rebuilding social skills, confidence, and relationships that have deteriorated during active addiction. The process can be challenging because it requires engaging socially while learning to navigate relationships without alcohol's temporary confidence and anxiety relief.
Support groups specifically for addiction recovery provide structured social environments where isolation can be addressed safely while maintaining sobriety. These groups offer opportunities to practice social engagement with others who understand the challenges of recovery and can provide encouragement and accountability for continued social participation.
Family therapy and relationship counseling often become necessary to repair the damage that anti-social behavior has caused to intimate relationships. Rebuilding trust, emotional availability, and authentic communication requires addressing the defensive patterns and avoidance behaviors that developed during active addiction.
Professional counseling can help address the underlying anxiety, depression, or other mental health issues that may have contributed to social withdrawal and continue to interfere with relationship building in recovery. Learning healthy coping strategies for social anxiety and developing genuine social skills becomes essential for maintaining long-term sobriety and rebuilding meaningful relationships.
Father Martin's identification of anti-social behavior as a cardinal symptom of alcoholism was crucial because it helped people understand that their social isolation and relationship difficulties were consequences of their drinking rather than character defects or unchangeable personality traits. By recognizing isolation as a symptom of the disease rather than a personal failing, individuals could begin to address these patterns systematically as part of their recovery process, ultimately rebuilding the social connections and community support that are essential for sustained sobriety and meaningful life in recovery.
The Progressive Nature of Relationship Deterioration:
Father Martin's identification of "loss of friends/family" as a symptom of alcoholism revealed one of the most heartbreaking and progressive consequences of alcohol dependency - the systematic erosion of the very relationships that provide meaning, support, and motivation for living. This symptom exposes how alcoholism doesn't just affect the individual, but radiates outward to damage and destroy the social fabric that normally sustains human wellbeing and provides natural intervention opportunities.
The loss of friends and family in alcoholism typically follows a predictable but tragic pattern that can span years or even decades. Father Martin understood that these relationship losses don't usually occur suddenly or dramatically, but rather through a gradual process of disappointment, boundary-setting, and eventual protective withdrawal by loved ones who can no longer tolerate the pain and unpredictability of maintaining relationships with someone whose behavior is increasingly dominated by alcohol.
The deterioration often begins with subtle changes in relationship dynamics that might not be immediately recognized as alcohol-related. Friends and family members may notice increased unreliability, mood swings, or defensive behavior, but may initially attribute these changes to stress, work pressures, or other life circumstances. The alcohol-related nature of these changes often becomes apparent only in retrospect, after patterns have been established and damage has accumulated.
Early relationship strain typically manifests as increased frequency of conflicts, misunderstandings, or disappointments related to alcohol-affected behavior. You might arrive late to events due to pre-drinking preparation, become argumentative or inappropriate during social gatherings, or fail to follow through on commitments made while drinking. These incidents create tension and confusion in relationships as loved ones struggle to understand why someone they care about is behaving inconsistently with their known character and values.
As alcoholism progresses, the incidents become more frequent and severe, creating a pattern of relationship stress that eventually overwhelms the natural resilience of even close relationships. Friends and family members find themselves walking on eggshells, making excuses for your behavior, or avoiding certain topics or situations that might trigger alcohol-related problems. The relationships gradually shift from mutual support and enjoyment to damage control and crisis management.
Stop Getting Invited Places - The Social Exclusion Process:
The cessation of social invitations represents one of the most painful and visible manifestations of how alcoholism affects relationships. This exclusion typically develops gradually as friends and family members learn from experience that including you in social events creates unpredictable stress and potential embarrassment for everyone involved.
The invitation withdrawal often begins with specific types of events rather than complete social exclusion. You might stop being invited to work-related social functions where professional behavior is important, family events where children will be present, or formal occasions where inappropriate behavior would be particularly embarrassing. These selective exclusions allow loved ones to maintain some relationship connection while protecting themselves and others from alcohol-related disruptions.
The process often involves careful calculation by friends and family about which events can safely include you and which cannot. They might consider factors like the duration of the event (longer events provide more opportunities for problems), the alcohol availability (events with unlimited alcohol might trigger excessive consumption), the social importance (important family milestones where disruption would be particularly painful), and the presence of vulnerable people (children, elderly relatives, or others who might be affected by inappropriate behavior).
The exclusion frequently becomes a topic of family discussion and planning that wouldn't have existed before alcohol became a problem. Family members might coordinate about whether to invite you to specific events, develop strategies for managing your behavior if you are invited, or create backup plans for handling problems that might arise. The energy and emotional resources devoted to these discussions represents a significant burden on family relationships and dynamics.
Business and professional exclusions often occur as colleagues learn that your presence at work-related social events creates risk for embarrassment or inappropriate behavior. You might stop being invited to office parties, business dinners, networking events, or professional conferences where alcohol is served. These exclusions can have serious career consequences, limiting networking opportunities and advancement possibilities while also creating professional isolation.
The exclusion process often involves painful conversations where friends or family members feel obligated to explain why you're not being invited to specific events. These conversations are typically awkward and distressing for everyone involved, as they require loved ones to acknowledge alcohol-related behavior problems while often encountering defensiveness, denial, or anger in response. Many people choose to avoid these conversations entirely, leading to unexplained exclusions that create additional confusion and resentment.
Didn't Want to Go to Events - The Self-Exclusion Pattern:
While external exclusion from social events is painful, the parallel process of self-exclusion is equally significant and often precedes or accompanies the withdrawal of invitations from others. The unwillingness to attend social events typically reflects the increasing incompatibility between alcohol dependency needs and normal social functioning requirements.
The self-exclusion often begins with events where alcohol consumption would be limited, monitored, or inappropriate. You might decline invitations to children's birthday parties where adult drinking is minimal, religious or spiritual gatherings where sobriety is expected, or health-focused activities where alcohol consumption would be conspicuous. These initial refusals seem reasonable and may not raise immediate concerns among friends and family.
As dependency deepens, the criteria for acceptable social events becomes increasingly narrow. You might find yourself only comfortable attending events specifically organized around drinking - happy hours, wine tastings, or parties where heavy alcohol consumption is normalized and expected. Social activities that don't center on drinking begin to feel pointless, anxiety-provoking, or impossible to enjoy without adequate alcohol preparation.
The self-exclusion frequently involves elaborate excuse generation to avoid explaining the real reasons for declining invitations. You might claim work obligations, health issues, financial constraints, or other commitments to avoid attending events where alcohol consumption would be problematic. These excuses often become increasingly implausible over time as the pattern of avoidance becomes more obvious to friends and family.
Anxiety about alcohol availability drives much of the self-exclusion behavior. You might decline invitations to events where you're uncertain about alcohol service, where you wouldn't be able to control consumption timing or quantity, or where your drinking patterns might be scrutinized by others. The fear of being in social situations without adequate alcohol access becomes more powerful than the desire for social connection and shared experiences.
The self-exclusion can extend to previously enjoyed activities that become incompatible with drinking routines or alcohol-affected functioning. Sporting events, concerts, theater performances, or other activities that require sustained attention or physical coordination might be avoided if they interfere with drinking schedules or reveal alcohol-related impairment.
Questioned About Being Under the Influence - The Scrutiny and Confrontation:
The experience of being questioned about intoxication represents a crucial turning point in relationship dynamics where alcohol-related behavior becomes too obvious to ignore or rationalize away. These confrontations often mark the transition from private concern to open acknowledgment that alcohol has become a visible problem affecting relationships and social functioning.
The questioning typically begins subtly, with friends or family members making indirect comments about your behavior, mood, or decision-making that suggest concern about alcohol influence. These might include observations about slurred speech, unsteady movement, inappropriate comments, or poor judgment that others attribute to drinking. The initial comments are often gentle and may be framed as concern rather than accusation.
As alcohol-related incidents become more frequent and obvious, the questioning becomes more direct and confrontational. Family members might ask directly whether you've been drinking, express concern about your alcohol consumption, or request that you not drink during specific events or conversations. These direct confrontations often trigger defensive responses, denial, or anger that further strain relationships.
The questioning often extends beyond specific incidents to broader patterns of behavior and lifestyle changes that family and friends attribute to alcohol influence. They might express concern about your reliability, judgment, health, or priorities in ways that implicitly or explicitly connect these concerns to drinking patterns. These conversations typically become increasingly difficult and emotionally charged as the gap between your perception and others' perceptions of your alcohol use becomes apparent.
Professional questioning can be particularly threatening because it involves career and financial security. Supervisors, colleagues, or clients might question whether alcohol is affecting your work performance, professional judgment, or business relationships. These professional confrontations often carry higher stakes and can motivate temporary behavior changes that don't address underlying dependency issues.
The pattern of being questioned creates a defensive mindset that can further damage relationships even when the questions are motivated by genuine concern and love. You might begin to see friends and family members as adversaries rather than allies, interpreting their concern as judgment, interference, or betrayal. This defensive stance often drives further isolation and relationship deterioration.
Only Talk to You When Sober - The Conditional Relationship Pattern:
The establishment of conditional communication patterns where friends and family only engage with you when you're sober represents a sophisticated boundary-setting strategy that attempts to maintain relationship connection while protecting against alcohol-related unpredictability and potential harm.
This conditional engagement often develops after repeated experiences where conversations or interactions during intoxication have led to problems, misunderstandings, or hurtful exchanges. Family members might learn that important discussions attempted while you're drinking are likely to be forgotten, misinterpreted, or result in conflict, leading them to postpone significant conversations until they're confident you're sober.
The timing strategies that family and friends develop around your drinking patterns can become quite sophisticated and burdensome. They might learn to recognize signs of intoxication, avoid calling during your typical drinking hours, or wait until morning to engage in serious conversations. This strategic communication management represents a significant accommodation to alcohol-related unpredictability that wouldn't be necessary in healthy relationships.
Children in families affected by alcoholism often naturally develop these conditional engagement patterns as a protective mechanism. They might learn to avoid approaching parents during drinking periods, wait until morning to discuss school problems or achievements, or develop the ability to assess intoxication levels before initiating interaction. These survival skills represent tragic adaptations that shouldn't be necessary in healthy family relationships.
The conditional communication often extends to emotional topics or important decisions that family members learn cannot be effectively addressed when alcohol is involved. Financial discussions, relationship issues, parenting decisions, or health concerns might be systematically postponed until sobriety can be assured. This creates artificial barriers to normal family functioning and decision-making processes.
Professional relationships may also develop conditional patterns where colleagues avoid important business discussions during times when alcohol influence is suspected. Client meetings might be rescheduled, important decisions might be postponed, or business communications might be limited to times when professional competence can be assured. These accommodations can have serious career consequences while also creating additional stress for professional relationships.
The Economic and Practical Consequences of Relationship Loss:
The loss of friends and family relationships due to alcoholism often creates significant practical and economic consequences that extend far beyond emotional pain. Social networks typically provide crucial support systems for employment opportunities, emergency assistance, childcare, financial help, and practical life management that become unavailable as relationships deteriorate.
Professional networking losses can have lasting career consequences as alcohol-related behavior damages relationships with colleagues, mentors, clients, and industry contacts. Job opportunities often come through personal relationships and professional networks that may be compromised by alcohol-related incidents or reputation damage. The loss of professional references, recommendations, and networking opportunities can create long-term economic disadvantage.
Family relationship deterioration often affects access to emergency support systems that most people take for granted. Financial emergencies, health crises, childcare needs, or housing problems typically rely on family assistance that may not be available when relationships have been damaged by alcohol-related behavior. The loss of these safety nets can create additional stress and crisis situations that drive further drinking.
Social relationship losses eliminate access to shared resources and mutual support systems that healthy friendships typically provide. Transportation assistance, childcare exchanges, home maintenance help, or emotional support during difficult times may no longer be available from friends who have withdrawn due to alcohol-related relationship damage. These practical losses compound the emotional pain of social isolation.
The Impact on Children and Family Dynamics:
The loss of friends and family relationships due to alcoholism has particularly devastating effects on children who lose not only parental emotional availability but also extended family and social connections that would normally provide additional support and stability.
Children often experience secondary relationship losses as alcohol-related family conflicts create tension with grandparents, aunts, uncles, and family friends who might otherwise provide important mentoring and support relationships. Family gatherings might be canceled or tense, holiday celebrations might be disrupted, and extended family relationships might become strained by alcohol-related incidents or conflicts.
The modeling of relationship dysfunction that children observe in families affected by alcoholism can affect their own social development and relationship skills. They might learn that relationships are unpredictable, that love is conditional on behavior, or that conflict and disappointment are normal aspects of close relationships. These lessons can affect their ability to form healthy relationships throughout their lives.
Friendships for children in families affected by alcoholism often suffer as parents become less available for the social coordination and hosting that typically supports children's social development. Playdates might be canceled, birthday parties might be missed, and parent-child social activities might be curtailed due to alcohol-related priorities or restrictions.
The Grief Process for Lost Relationships:
Family members and friends who withdraw from relationships due to alcohol-related behavior often experience a complex grief process that involves mourning the loss of the person they knew before alcohol became dominant while simultaneously protecting themselves from ongoing harm and disappointment.
The grief typically involves anger at the alcohol-related behavior changes, sadness about the loss of relationship connection, guilt about setting boundaries or withdrawing support, and hope that the person might eventually address their alcohol problems and relationships might be restored. This complex emotional process can last for years and significantly affect the mental health and wellbeing of family members and friends.
The ambiguous loss that families experience when someone is physically present but emotionally unavailable due to alcohol can be particularly difficult to process. Unlike death or clear relationship endings, the ongoing possibility of recovery and relationship restoration creates uncertainty about how to grieve and move forward. Family members might struggle with questions about how much support to provide, when to establish boundaries, and whether to maintain hope for change.
Support groups for family members affected by alcoholism often focus heavily on processing this relationship grief and learning healthy ways to maintain emotional wellbeing while a loved one struggles with alcohol dependency. The recognition that loving someone doesn't require accepting harmful behavior becomes crucial for family members' ability to protect their own mental health and model healthy boundaries.
The Potential for Relationship Restoration:
While the loss of friends and family relationships represents one of the most painful consequences of alcoholism, Father Martin also understood that recovery creates opportunities for relationship restoration and renewal that can be profoundly meaningful for both the person in recovery and their loved ones.
The process of making amends, taking responsibility for alcohol-related relationship damage, and demonstrating sustained behavior change can gradually rebuild trust and connection with family members and friends who have been hurt by alcohol-related behavior. However, this process typically requires patience, consistency, and recognition that others have been legitimately harmed and may need time to trust again.
Some relationships may not survive the damage caused by alcohol-related behavior, and recovery often involves accepting this loss while working to prevent future relationship damage. The grief process for permanently lost relationships becomes part of recovery work, alongside the commitment to protecting current and future relationships from alcohol-related harm.
New relationships formed in recovery often have different characteristics than pre-alcoholism relationships because they're built on foundations of honesty, vulnerability, and shared commitment to healthy living rather than social drinking or denial of problems. These relationships can provide models for healthier connection and support recovery maintenance.
The Relationship Between Isolation and Recovery:
Father Martin recognized that the relationship losses caused by alcoholism create both barriers to recovery (through isolation and loss of support systems) and motivation for recovery (through the pain of lost connections and desire to rebuild relationships). The social consequences often provide crucial motivation for seeking treatment when other consequences might be easier to deny or rationalize.
Recovery typically requires rebuilding social skills and confidence that may have deteriorated during active alcoholism. Learning to interact socially without alcohol, developing genuine intimacy and communication skills, and rebuilding trust with loved ones becomes essential recovery work that extends far beyond stopping drinking.
The reconstruction of healthy relationships often serves as both a goal and a measure of recovery progress. The ability to maintain consistent, honest, and supportive relationships becomes evidence of sustained recovery and emotional health that extends beyond alcohol consumption patterns.
Father Martin's identification of friend and family loss as a cardinal symptom of alcoholism was crucial because it helped people understand that their social isolation and relationship problems were consequences of their drinking rather than evidence that they were fundamentally unlovable or antisocial. By recognizing relationship deterioration as a symptom of the disease, individuals could begin to address these patterns through recovery work while also understanding that relationship restoration would be possible with sustained sobriety and commitment to making amends for past harm.
The Progressive Medical Deterioration of Alcoholism:
Father Martin's identification of "hospitals or medical support" as a symptom of alcoholism revealed one of the most serious and progressive consequences of alcohol dependency - the systematic deterioration of physical health and the increasing need for medical intervention to address alcohol-related health crises. This symptom represents the point where alcoholism transitions from a behavioral or psychological problem to a life-threatening medical condition requiring professional intervention and ongoing healthcare management.
The medical consequences of alcoholism typically develop gradually over years or decades, often remaining hidden or misattributed to other causes until they reach crisis proportions. Father Martin understood that alcohol's effects on virtually every organ system in the body create a cascade of health problems that eventually become impossible to ignore or manage without professional medical intervention.
The progression often begins with subtle symptoms that might be dismissed as normal aging, stress-related problems, or minor health issues unrelated to alcohol consumption. Early symptoms might include fatigue, sleep disturbances, digestive problems, frequent infections, or minor injuries that heal slowly. These early warning signs are often rationalized away or attributed to work stress, poor diet, lack of exercise, or other lifestyle factors while alcohol consumption continues to increase.
As alcoholism progresses, the symptoms become more severe and obviously health-related, eventually requiring medical attention that may reveal alcohol as the underlying cause. Blood tests might show elevated liver enzymes, blood pressure readings might reveal hypertension, or routine examinations might uncover early signs of organ damage. At this stage, honest communication with healthcare providers becomes crucial for proper diagnosis and treatment, but shame and denial often interfere with accurate reporting of alcohol consumption levels.
The medical progression of alcoholism often follows predictable patterns that reflect alcohol's toxic effects on specific organ systems. However, the timeline and severity can vary dramatically based on individual factors including genetics, overall health, nutrition, concurrent medical conditions, and the duration and intensity of alcohol consumption.
Liver Disease - The Most Visible Organ Damage:
Liver damage represents the most well-known and feared medical consequence of alcoholism because the liver bears primary responsibility for metabolizing alcohol and is therefore exposed to alcohol's toxic effects with every drink consumed. The progression of alcohol-related liver disease typically follows distinct stages that can be identified through medical testing and may be reversible if alcohol consumption stops early enough in the process.
Fatty liver disease represents the earliest stage of alcohol-related liver damage and can develop after relatively short periods of heavy drinking. This condition involves the accumulation of fat deposits in liver cells, which can impair liver function and create symptoms including fatigue, abdominal discomfort, and elevated liver enzyme levels in blood tests. Fatty liver disease is often reversible with abstinence from alcohol, but continued drinking leads to more serious liver damage.
Alcoholic hepatitis represents a more advanced stage of liver damage involving inflammation and cell death that can cause serious symptoms including jaundice (yellowing of skin and eyes), severe fatigue, abdominal pain, nausea, and appetite loss. This condition can be life-threatening and requires immediate medical attention and complete abstinence from alcohol. Some people develop alcoholic hepatitis after relatively short periods of heavy drinking, while others may drink heavily for years without developing this condition.
Cirrhosis represents the most advanced and irreversible stage of alcohol-related liver damage, involving permanent scarring that prevents the liver from functioning properly. Symptoms can include swelling in legs and abdomen, confusion and cognitive impairment, bleeding problems, and eventual liver failure. Cirrhosis significantly increases the risk of liver cancer and can only be treated through liver transplantation in end-stage cases. Even with abstinence, cirrhosis damage cannot be reversed, though further progression can be prevented.
The psychological impact of liver disease diagnosis can be profound, often serving as a wake-up call that motivates attempts at alcohol reduction or cessation. However, the advanced stages of liver disease can also create feelings of hopelessness and despair that paradoxically drive continued drinking as a coping mechanism for facing a potentially terminal diagnosis.
Cardiovascular Disease - The Hidden Heart Damage:
Alcohol's effects on the cardiovascular system are complex and often overlooked compared to liver damage, but they can be equally serious and life-threatening. Heavy alcohol consumption affects the heart, blood vessels, and blood pressure in ways that significantly increase the risk of heart disease, stroke, and sudden cardiac death.
Alcoholic cardiomyopathy involves the weakening and enlargement of heart muscle due to alcohol's toxic effects, leading to reduced pumping efficiency and potential heart failure. This condition can develop silently over years of heavy drinking and may not cause obvious symptoms until heart function is significantly compromised. Symptoms can include shortness of breath, fatigue, swelling in legs and feet, and irregular heartbeat patterns.
Hypertension (high blood pressure) is commonly associated with heavy alcohol consumption and significantly increases the risk of stroke, heart attack, and kidney disease. Alcohol's effects on blood pressure can be both acute (temporary increases during drinking episodes) and chronic (persistently elevated blood pressure due to long-term alcohol use). The hypertension often requires medication management even after alcohol cessation.
Arrhythmias (irregular heart rhythms) can be triggered by both acute alcohol consumption and chronic alcohol use, potentially leading to sudden cardiac death even in relatively young people without obvious heart disease. "Holiday heart syndrome" describes arrhythmias that occur after binge drinking episodes, while chronic alcohol use can create persistent rhythm problems that require ongoing cardiac monitoring and treatment.
Stroke risk is significantly elevated in people with alcoholism due to alcohol's effects on blood pressure, blood clotting, and blood vessel health. Both bleeding strokes (caused by ruptured blood vessels) and clotting strokes (caused by blocked blood vessels) are more common in heavy drinkers, and the risk remains elevated even after alcohol cessation due to permanent blood vessel damage.
Accidents and Injuries - The Immediate Physical Dangers:
Alcohol-related accidents and injuries represent some of the most dramatic and immediately visible consequences of alcoholism, often serving as crisis points that force recognition of alcohol-related problems and may motivate attempts at treatment. These incidents can range from minor injuries to life-threatening trauma that requires emergency medical intervention and extended hospitalization.
Motor vehicle accidents represent the most serious and well-known category of alcohol-related injuries, involving not only the risk to the intoxicated driver but also innocent passengers, other drivers, and pedestrians. Alcohol impairs reaction time, judgment, coordination, and vision in ways that dramatically increase accident risk even at relatively low blood alcohol levels. The legal, financial, and psychological consequences of alcohol-related vehicle accidents can be devastating and life-altering.
Falls represent the most common type of alcohol-related injury, particularly among older adults whose balance and coordination are already compromised by aging. Alcohol-related falls can result in head injuries, broken bones, cuts, and bruises that require emergency medical treatment. Repeated falls often alert family members and healthcare providers to potential alcohol problems, especially when injuries seem disproportionate to reported circumstances.
Burns and cuts are common alcohol-related injuries that occur due to impaired coordination and judgment around cooking, smoking, tools, or other potentially dangerous activities. These injuries might seem minor individually but can create patterns that reveal alcohol-related impairment to healthcare providers, family members, or employers. Severe burns or cuts may require emergency treatment, surgery, or extended wound care.
Violent injuries can result from alcohol-related altercations, domestic violence, or other conflicts that escalate due to alcohol's effects on aggression and judgment. These injuries may involve police reports, legal consequences, and protective orders that create additional stress and complications beyond the immediate medical treatment needs.
Work-related injuries often increase in frequency and severity among people with alcoholism due to impaired coordination, judgment, and reaction time in workplace settings. These injuries can result in workers' compensation claims, job loss, and disability that create additional financial and psychological stress while also revealing alcohol problems to employers and insurance companies.
Emergency Department Utilization Patterns:
People with alcoholism often develop patterns of emergency department utilization that reflect both acute alcohol-related crises and the general health deterioration associated with chronic alcohol use. Emergency departments become familiar with frequent visitors whose repeated presentations follow alcohol-related patterns.
Acute intoxication episodes may require emergency medical treatment for alcohol poisoning, which can be life-threatening and requires immediate intervention to prevent coma, respiratory depression, or death. These episodes often involve extremely high blood alcohol levels that require medical monitoring and supportive care until the alcohol is metabolized and eliminated from the system.
Withdrawal symptoms can create medical emergencies requiring immediate professional intervention, particularly when they progress to delirium tremens (DTs), which involves confusion, hallucinations, severe agitation, and potentially life-threatening changes in heart rate and blood pressure. Alcohol withdrawal can be more dangerous than withdrawal from many other substances and often requires hospitalization for safe medical management.
Blackout-related injuries frequently bring people to emergency departments when they wake up with unexplained injuries, wounds, or physical symptoms that occurred during memory blackouts. These presentations often involve detective work to determine what happened and whether serious injuries or medical conditions require immediate treatment.
Psychiatric emergencies related to alcohol use can include suicide attempts, severe depression, anxiety attacks, or psychotic episodes that require immediate mental health intervention. The combination of alcohol's depressant effects and the life problems created by alcoholism can precipitate serious mental health crises requiring emergency psychiatric evaluation and treatment.
Gastrointestinal Complications:
Alcohol's effects on the digestive system create numerous health problems that often require medical intervention and can become life-threatening if alcohol consumption continues. These complications affect every part of the digestive tract from the mouth and esophagus to the intestines and pancreas.
Gastritis and peptic ulcers are common complications of heavy alcohol use that can cause severe abdominal pain, nausea, vomiting, and potentially life-threatening bleeding. The combination of alcohol's direct irritating effects on stomach lining and its interaction with stomach acid creates erosions and ulcers that may require emergency treatment and ongoing medical management.
Pancreatitis is a serious and potentially fatal complication of alcoholism involving inflammation of the pancreas that causes severe abdominal pain, vomiting, and potential organ failure. Acute pancreatitis often requires hospitalization for pain management and supportive care, while chronic pancreatitis can lead to diabetes and ongoing digestive problems that require lifelong medical management.
Esophageal varices represent a life-threatening complication of advanced liver disease where enlarged blood vessels in the esophagus can rupture and cause massive, potentially fatal bleeding. This condition requires emergency medical intervention and ongoing monitoring for people with alcohol-related liver cirrhosis.
Malnutrition and vitamin deficiencies are common in alcoholism due to alcohol's interference with nutrient absorption and the tendency for alcohol to replace food calories. Severe deficiencies can cause neurological problems, anemia, and immune system dysfunction that require medical treatment and nutritional rehabilitation.
Neurological and Cognitive Complications:
Alcohol's effects on the brain and nervous system create numerous health problems that often require specialized medical treatment and can result in permanent disability if alcohol consumption continues. These complications affect both cognitive functioning and physical neurological abilities.
Wernicke-Korsakoff syndrome is a serious neurological condition caused by thiamine (vitamin B1) deficiency common in alcoholism. Wernicke's encephalopathy involves confusion, coordination problems, and eye movement abnormalities that require immediate medical treatment to prevent progression to Korsakoff's psychosis, which involves severe memory problems and confabulation that may be irreversible.
Peripheral neuropathy involves damage to nerves in hands and feet that causes numbness, tingling, pain, and weakness that can significantly affect daily functioning. This condition often develops gradually and may be partially reversible with alcohol cessation and nutritional rehabilitation, but advanced cases can cause permanent disability.
Alcoholic dementia involves progressive cognitive decline that can affect memory, judgment, problem-solving, and daily living skills. While some cognitive improvement may occur with sustained abstinence, advanced alcoholic dementia can cause permanent intellectual disability requiring ongoing care and support.
Seizures can occur both during acute alcohol withdrawal and as a result of chronic brain damage from long-term alcohol use. Alcohol-related seizures often require emergency medical treatment and ongoing neurological monitoring to prevent additional seizures and brain injury.
Mental Health Treatment Integration:
The medical treatment of alcoholism increasingly involves integrated approaches that address both the physical health consequences and the underlying psychological factors that drive continued alcohol use. This integration reflects growing recognition that alcoholism is a complex medical condition requiring comprehensive treatment rather than simply addressing individual symptoms or complications.
Psychiatric evaluation and treatment often become necessary components of medical care for alcoholism, particularly when depression, anxiety, trauma, or other mental health conditions contribute to alcohol use or complicate recovery efforts. The high rates of co-occurring mental health disorders among people with alcoholism require specialized treatment approaches that address both conditions simultaneously.
Medication-assisted treatment for alcoholism has evolved to include medications that reduce alcohol cravings, block alcohol's euphoric effects, or create unpleasant reactions when alcohol is consumed. These medications require medical supervision and ongoing monitoring but can significantly improve treatment outcomes when combined with counseling and behavioral interventions.
Addiction medicine specialists have emerged as medical professionals specifically trained to address the complex health needs of people with substance use disorders, providing comprehensive care that addresses both acute medical complications and long-term recovery support.
Treatment and Rehabilitation Services:
The medical treatment of alcoholism has evolved far beyond simple detoxification to include comprehensive rehabilitation services that address the multiple dimensions of recovery needed for sustained sobriety and health restoration. These services often involve extended treatment periods and ongoing medical support.
Medically supervised detoxification provides safe management of alcohol withdrawal symptoms in controlled healthcare settings where complications can be immediately addressed. This process often requires several days of medical monitoring and medication management to prevent serious withdrawal complications while beginning the recovery process.
Inpatient rehabilitation programs provide intensive medical and psychological treatment in residential settings where people can focus entirely on recovery without the distractions and triggers of daily life. These programs typically last 30-90 days and include medical monitoring, individual and group counseling, education about addiction, and planning for ongoing outpatient care.
Outpatient treatment programs allow people to receive addiction treatment while maintaining work, family, and other life responsibilities. These programs can range from intensive daily treatment to weekly counseling sessions, with medical monitoring and support provided as needed for ongoing health issues related to alcohol use.
Halfway houses and sober living facilities provide transitional housing with ongoing support and accountability for people in early recovery who need structured environments but are ready for increased independence. These facilities often include medical support and coordination with healthcare providers for ongoing treatment of alcohol-related health problems.
The Role of Healthcare Provider Recognition:
Healthcare providers play a crucial role in identifying and addressing alcoholism before it progresses to life-threatening complications. However, this recognition often depends on honest communication from patients about their alcohol consumption, which shame and denial frequently prevent.
Routine medical screening for alcohol use has become standard practice in many healthcare settings, with healthcare providers trained to recognize signs of alcohol-related health problems and ask appropriate questions about drinking patterns. These screening efforts can identify alcohol problems earlier and connect people with appropriate treatment resources.
Emergency department protocols increasingly include alcohol screening and brief intervention services that can provide immediate motivation and resources for people presenting with alcohol-related injuries or health problems. These interventions often occur during moments of crisis when people may be more receptive to recognizing alcohol-related problems and considering treatment.
Primary care integration of addiction treatment services allows for ongoing medical management of alcohol-related health problems while also providing support for recovery efforts. This integrated approach recognizes that alcoholism is a chronic medical condition requiring long-term management rather than a short-term treatment episode.
The Economic Impact of Medical Consequences:
The medical consequences of alcoholism create enormous economic burdens for individuals, families, and healthcare systems that often motivate recognition of alcohol problems and attempts at treatment. These costs can accumulate rapidly and create financial crises that compound other alcohol-related problems.
Emergency department visits, hospitalizations, surgeries, and ongoing medical treatments for alcohol-related health problems can result in overwhelming medical bills that create financial devastation for individuals and families. Even with health insurance, the co-pays, deductibles, and uncovered services can create substantial financial burden.
Lost work time due to alcohol-related illnesses, injuries, and medical treatments often compounds the financial impact by reducing income while medical expenses increase. Disability claims related to alcohol-related health problems may provide some income replacement but typically at reduced levels that create additional financial stress.
Health insurance complications can arise when alcohol-related health problems are identified, potentially affecting coverage decisions, premium costs, or policy renewability. Some insurance policies have specific exclusions or limitations for alcohol-related medical expenses, creating additional financial burden for treatment costs.
Long-term Medical Monitoring and Management:
Recovery from alcoholism often requires ongoing medical monitoring and management of alcohol-related health problems that may persist even after alcohol cessation. This long-term medical care represents a significant component of comprehensive recovery planning and support.
Liver function monitoring through regular blood tests and imaging studies becomes necessary for people with alcohol-related liver damage to assess recovery progress and monitor for complications. Some liver damage may be reversible with sustained abstinence, while other damage requires ongoing management and monitoring for progression.
Cardiovascular health monitoring includes regular blood pressure checks, heart function assessments, and screening for complications related to alcohol-related heart damage. Medications may be needed to manage blood pressure, heart rhythm problems, or other cardiovascular consequences that persist after alcohol cessation.
Nutritional rehabilitation often requires ongoing medical support to address deficiencies created by alcohol's interference with nutrition and to support physical recovery from alcohol-related organ damage. This may include vitamin supplementation, dietary counseling, and monitoring of nutritional status during recovery.
Mental health follow-up becomes crucial for addressing ongoing psychological effects of alcohol use and any co-occurring mental health conditions that may affect recovery success. This ongoing mental health support helps prevent relapse and addresses the emotional and psychological challenges of sustained recovery.
Father Martin's identification of medical consequences as a key symptom of alcoholism was crucial because it helped people understand that their health problems might be directly related to their alcohol consumption and that medical intervention could be both necessary for addressing immediate health crises and helpful for supporting long-term recovery efforts. By recognizing the serious medical nature of alcoholism, individuals could begin to approach their drinking problems as health issues requiring professional treatment rather than personal failings requiring only willpower and determination. This medical framework often provides the motivation and resources necessary for sustained recovery while also addressing the serious health consequences that may have accumulated during active addiction.
The Psychology and Physiology of Binge Drinking in Alcoholism:
Father Martin's identification of "binges or benders" as a symptom of alcoholism revealed one of the most dangerous and psychologically revealing patterns of alcohol consumption - the compulsive, extended drinking episodes that demonstrate complete loss of control and represent some of the highest-risk periods for alcohol-related death, injury, and life-threatening complications. This symptom exposes how alcoholism can manifest not just as daily heavy drinking, but as periodic episodes of extreme consumption that can be equally or more destructive than consistent daily drinking patterns.
Binges and benders represent a distinct pattern of alcoholism that differs fundamentally from steady, daily heavy drinking. Father Martin understood that these episodes reflect a complex interplay of psychological compulsion, physiological tolerance, and behavioral disinhibition that creates self-perpetuating cycles of extreme alcohol consumption lasting days, weeks, or even months.
The binge pattern often develops in people who attempt to control their drinking through periods of abstinence or moderation, only to find that when they do drink, they cannot stop until physical collapse, external intervention, or complete depletion of alcohol supplies forces cessation. This pattern creates a false sense of control during abstinent periods while actually demonstrating profound loss of control when alcohol consumption begins.
The physiological aspects of binge drinking involve rapid increases in blood alcohol concentration that overwhelm the body's ability to metabolize alcohol safely. During extended benders, the person may maintain continuously high blood alcohol levels for days or weeks, creating serious risks for alcohol poisoning, dehydration, malnutrition, and medical complications that can be life-threatening.
Psychologically, binges often involve a complete abandonment of normal responsibilities, relationships, and self-care in favor of continued alcohol consumption. The person may disappear from work, family, and social obligations for extended periods, emerging from the binge with significant damage to relationships, employment, health, and financial stability.
The binge pattern frequently involves a buildup of psychological pressure during periods of abstinence or controlled drinking, followed by explosive release through extreme consumption. This pressure-cooker dynamic creates a cycle where attempts at moderation actually contribute to the severity of eventual binge episodes.
"Catching Up on Lost Time" - The Compensatory Drinking Phenomenon:
The concept of "catching up on lost time" reveals one of the most psychologically sophisticated aspects of binge drinking in alcoholism - the belief that periods of abstinence or reduced drinking create a deficit that must be compensated through intensified consumption. This mindset transforms drinking from a pleasurable activity into a compulsive effort to make up for perceived lost opportunities for intoxication.
The catch-up mentality often develops in people who attempt to control their drinking through temporal restrictions - only drinking on weekends, avoiding alcohol during work weeks, or abstaining during periods of high responsibility. However, rather than reducing overall consumption, these restrictions often lead to compensatory binge drinking that results in higher total alcohol intake and more dangerous consumption patterns.
The psychology behind catch-up drinking involves treating alcohol consumption as if it were a commodity that can be stockpiled or banked. The person may calculate how many drinks they "missed" during abstinent periods and attempt to consume equivalent amounts during binges. This mathematical approach to drinking reveals the extent to which alcohol has become a central organizing principle in their thinking and planning.
Weekend benders often represent the most common form of catch-up drinking, where people who maintain sobriety during work weeks engage in extreme consumption from Friday evening through Sunday night. These episodes may involve consuming a week's worth of alcohol in two or three days, creating dangerous spikes in blood alcohol concentration and significant physical and psychological stress.
Holiday and vacation binges frequently involve the belief that special occasions justify or require extreme drinking to "make up for" periods of responsible behavior. The person may view vacations, holidays, or celebrations as opportunities to indulge in the level of drinking they believe they've been deprived of during normal life periods.
The catch-up phenomenon often involves elaborate planning and anticipation that reveals the central role alcohol has assumed in the person's mental life. They may spend weeks planning drinking binges, researching alcohol availability at destinations, or calculating optimal consumption strategies to maximize intoxication during limited time periods.
"Trying to Get It All In at Once" - The Urgency and Desperation of Binge Consumption:
The compulsion to "get it all in at once" reflects the desperate urgency that characterizes binge drinking episodes, where the person attempts to achieve maximum intoxication as quickly as possible, often consuming dangerous quantities of alcohol in compressed time periods. This pattern reveals both the intensity of alcohol craving and the awareness that the drinking opportunity may be limited or interrupted.
The urgency often stems from awareness that the binge period is temporary and will eventually end due to external pressures, responsibilities, or physical limitations. This creates a frantic quality to the drinking where the person attempts to consume as much alcohol as possible before circumstances force cessation. The drinking becomes less about enjoyment and more about desperate stockpiling of intoxication effects.
Speed of consumption during binges often reaches dangerous levels as the person prioritizes rapid alcohol absorption over taste, social interaction, or physical comfort. They may switch to higher-proof alcohol, drink without eating, or consume alcohol in ways specifically designed to maximize absorption speed and intoxication intensity.
The "all at once" mentality often involves abandoning normal drinking rituals and social conventions in favor of efficient alcohol delivery. The person may drink directly from bottles rather than using glasses, consume alcohol first thing in the morning to maintain or achieve intoxication, or mix different types of alcohol without regard for taste or traditional drinking customs.
Hoarding behavior often accompanies the urgency to consume everything immediately. The person may purchase large quantities of alcohol at the beginning of binges, creating stockpiles designed to prevent interruption of consumption. This hoarding reveals the fear that alcohol access might be limited and the determination to maintain consumption regardless of external circumstances.
The desperation quality of "getting it all in" often involves overriding physical discomfort, nausea, or other bodily signals that would normally limit consumption. The person may continue drinking despite vomiting, stomach pain, or obvious intoxication symptoms because the psychological drive to maximize consumption overrides physical self-preservation instincts.
"Can't Stop for Days" - The Loss of Control and Extended Duration:
The inability to stop drinking for days or weeks represents the most serious manifestation of binge drinking and demonstrates complete loss of voluntary control over alcohol consumption. This pattern shows how alcoholism can involve not just difficulty moderating drinking, but complete inability to cease consumption once it begins, regardless of consequences or external pressures.
The extended duration of benders often surprises even the person experiencing them, as initial intentions to drink for limited periods extend indefinitely due to the inability to stop voluntarily. What begins as planned weekend drinking may continue for weeks or months, consuming vacation time, sick leave, and eventually resulting in job loss or other serious consequences.
Physical dependence often develops rapidly during extended benders as the body adapts to continuously high alcohol levels and begins experiencing withdrawal symptoms whenever blood alcohol concentration drops. This creates a physiological drive to continue drinking that reinforces the psychological compulsion, making cessation increasingly difficult without medical intervention.
The daily structure during benders typically revolves entirely around alcohol consumption and procurement, with all other activities becoming secondary to maintaining intoxication. Normal self-care, hygiene, nutrition, and social interaction are abandoned in favor of continued drinking, often resulting in serious physical deterioration and health complications.
Sleep patterns during extended benders often become severely disrupted as alcohol interferes with normal sleep cycles while simultaneously being used to manage withdrawal symptoms that emerge during brief periods of reduced consumption. The person may experience a cycle of drinking to sleep, waking in withdrawal, and drinking to relieve withdrawal symptoms.
Financial consequences of extended benders can be devastating as normal budgeting and financial responsibility are abandoned in favor of continued alcohol procurement. Credit cards may be maxed out, savings depleted, or valuable possessions sold to maintain alcohol supplies during extended drinking episodes.
The Bender Cycle - Buildup, Explosion, and Recovery:
Extended drinking binges typically follow predictable cycles that can span weeks, months, or even years, with each phase presenting distinct psychological and behavioral characteristics. Understanding this cycle helps explain how binge drinking differs from other patterns of alcoholism and why it can be particularly difficult to interrupt or treat.
The buildup phase often involves increasing psychological pressure and tension as the person attempts to maintain abstinence or controlled drinking despite growing cravings and obsessive thoughts about alcohol. This period may last days, weeks, or months, during which the person may appear to be functioning normally while internally struggling with intense desire to drink.
During buildup periods, triggers often accumulate and intensify, including stress from work or relationships, anniversary dates associated with previous drinking episodes, exposure to alcohol-related cues, or simply the passage of time since the last drinking episode. These triggers create mounting pressure that eventually overwhelms whatever control mechanisms the person has developed.
The explosion phase represents the actual beginning of the binge, often triggered by a specific event, emotional crisis, or simply reaching a psychological breaking point where the pressure to drink becomes irresistible. The initial drinking during this phase often occurs with full awareness that it will likely lead to an extended binge, yet the person feels powerless to prevent or control the progression.
The active binge phase involves complete surrender to alcohol consumption, with all normal responsibilities and activities abandoned in favor of continued drinking. This phase may last days, weeks, or months, during which the person becomes increasingly isolated, physically deteriorated, and consumed with maintaining alcohol supplies and consumption.
The crash phase occurs when external circumstances force cessation of drinking - complete depletion of financial resources, physical collapse requiring medical intervention, legal consequences, or intervention by family members or employers. This phase often involves severe withdrawal symptoms, medical complications, and overwhelming shame and remorse about the behavior during the binge.
The recovery phase involves gradual physical and psychological stabilization as withdrawal symptoms subside and the person begins to assess and address the damage caused during the binge episode. This phase often includes promises to never drink again, attempts to repair damaged relationships and responsibilities, and renewed commitment to maintaining sobriety.
Trigger Events and Environmental Factors:
Binge drinking episodes rarely occur randomly but are typically triggered by specific events, emotional states, or environmental factors that overwhelm the person's ability to maintain abstinence or controlled drinking. Understanding these triggers becomes crucial for prevention and treatment of binge drinking patterns.
Emotional triggers often involve overwhelming stress, grief, anger, or other intense feelings that the person lacks healthy coping mechanisms to manage. Relationship conflicts, work pressures, financial problems, or family crises can precipitate binge episodes as the person seeks to escape or numb emotional pain through alcohol consumption.
Anniversary reactions represent a common trigger where specific dates associated with traumatic events, losses, or previous drinking episodes create psychological vulnerability that leads to binge drinking. These may include death anniversaries, divorce dates, job loss dates, or anniversaries of previous rock-bottom experiences that create emotional distress.
Social triggers can include exposure to drinking environments, contact with drinking companions, or social pressures that overwhelm the person's ability to maintain sobriety. Weddings, reunions, parties, or other social events where alcohol is prominent may trigger binge episodes in people who have been maintaining abstinence.
Environmental cues such as passing familiar bars, finding hidden alcohol supplies, or even seeing alcohol advertisements can trigger intense cravings that lead to binge episodes. The power of these environmental triggers often surprises people in recovery and demonstrates the importance of environmental management in preventing relapse.
Success paradox represents a counterintuitive trigger where positive events such as job promotions, relationship milestones, or recovery anniversaries create anxiety or feelings of unworthiness that precipitate binge drinking. The fear of success or belief that good things don't last can sabotage progress and trigger self-destructive drinking episodes.
The Physical Dangers of Extended Binges:
Binge drinking and extended benders represent some of the most physically dangerous patterns of alcohol consumption, with risks for life-threatening complications that increase dramatically with the duration and intensity of drinking episodes. The concentrated nature of binge consumption creates acute medical risks that may not be present with steady daily drinking patterns.
Alcohol poisoning represents the most immediate and serious risk during binge episodes, as rapid consumption can lead to blood alcohol concentrations that suppress vital bodily functions including breathing and heart rate. Unlike gradual drinking where tolerance may provide some protection, binge drinking often involves consuming alcohol faster than tolerance can accommodate.
Dehydration and electrolyte imbalances commonly occur during extended binges as alcohol's diuretic effects combine with poor nutrition and fluid intake to create dangerous chemical imbalances in the body. These imbalances can affect heart rhythm, muscle function, and neurological activity, potentially leading to seizures, cardiac arrhythmias, or other life-threatening complications.
Malnutrition develops rapidly during extended benders as alcohol calories replace food calories and alcohol interferes with nutrient absorption. Severe nutritional deficiencies can develop within days or weeks, affecting immune function, wound healing, and neurological functioning. Thiamine deficiency is particularly dangerous and can lead to irreversible brain damage if not treated promptly.
Withdrawal complications become increasingly severe with longer binge duration as the body becomes adapted to continuously high alcohol levels. Sudden cessation after extended binges can precipitate life-threatening withdrawal symptoms including seizures, delirium tremens, and cardiovascular instability that require immediate medical intervention.
Accident and injury risks are dramatically elevated during binge episodes due to severe intoxication combined with impaired judgment about risk assessment. Falls, burns, cuts, and other injuries are common during binges, and the severity may be increased by alcohol's effects on bleeding and healing processes.
The Social and Occupational Consequences:
Extended drinking binges often result in some of the most severe and immediate social and occupational consequences of alcoholism, as the complete abandonment of responsibilities during binge episodes creates crises that are difficult to explain or repair. These consequences often serve as wake-up calls that motivate treatment seeking.
Employment consequences can be devastating when binges result in extended unexplained absences, missed deadlines, or obvious intoxication at work. Unlike gradual performance decline associated with daily drinking, binge-related work problems often result in immediate disciplinary action or termination due to the dramatic nature of the behavior change.
Family relationships suffer severe strain when binges result in complete disappearance or unavailability during important family events, emergencies, or daily responsibilities. Spouses may be left to handle all family responsibilities alone while also worrying about the safety and wellbeing of the person on the binge.
Financial consequences can be catastrophic when binges involve spending large amounts of money on alcohol over short periods, often depleting savings, maxing out credit cards, or selling valuable possessions to maintain drinking. The concentrated nature of binge spending can create immediate financial crises rather than gradual financial decline.
Legal problems often result from binge episodes due to driving under the influence, public intoxication, domestic violence, or other alcohol-related offenses that occur during periods of extreme intoxication. The severity of intoxication during binges often leads to more serious charges and consequences than might occur with lower-level daily drinking.
The Psychological Profile of Binge Drinkers:
People who engage in binge drinking often have distinct psychological characteristics that differentiate them from steady daily drinkers, though both patterns represent serious forms of alcoholism requiring professional treatment. Understanding these differences can be important for developing appropriate treatment strategies.
All-or-nothing thinking patterns are common among binge drinkers, who often struggle with moderation in many areas of life beyond alcohol consumption. This cognitive style may contribute to the belief that complete abstinence is impossible, making binge episodes seem inevitable when any alcohol consumption occurs.
Perfectionism and control issues often characterize people with binge drinking patterns, who may maintain strict control over alcohol consumption for extended periods before experiencing complete loss of control during binge episodes. The contrast between periods of rigid control and complete abandonment can be psychologically devastating.
Emotional regulation difficulties frequently underlie binge drinking patterns, as people may use alcohol to manage intense emotions that feel overwhelming or unmanageable through other means. The binge pattern may represent an attempt to completely escape emotional pain rather than gradually managing it.
Trauma history is common among people with binge drinking patterns, with binges often serving as attempts to numb or escape traumatic memories, anniversary reactions, or post-traumatic stress symptoms. The intensity of binge drinking may reflect the severity of underlying trauma requiring specialized treatment.
Treatment Considerations for Binge Drinking Patterns:
Treating binge drinking requires specialized approaches that address both the acute medical risks of binge episodes and the underlying psychological factors that drive the binge cycle. Traditional addiction treatment approaches may need modification to address the unique characteristics of binge drinking patterns.
Medical stabilization often requires immediate attention when people seek treatment during or immediately after binge episodes, as withdrawal symptoms can be severe and potentially life-threatening. Medical detoxification may be more complex and require longer monitoring periods than for steady daily drinkers.
Crisis intervention skills become crucial for people with binge drinking patterns, who need strategies for managing triggers and preventing binges rather than simply reducing daily consumption. Treatment often focuses on developing alternative coping strategies for emotional crises that typically precipitate binge episodes.
Relapse prevention for binge drinkers must address the unique aspects of the binge cycle, including recognizing buildup phases, managing triggers, and developing emergency intervention strategies for high-risk periods. The extended abstinence periods between binges can create false confidence that the problem is resolved.
Family involvement often requires specialized approaches because family members may experience relief during abstinent periods followed by crisis during binge episodes. Family therapy must address the unique stress patterns created by binge drinking cycles and help develop appropriate responses to binge episodes.
The Relationship Between Binges and Recovery:
Binge drinking patterns often create unique challenges and opportunities in recovery, as the dramatic nature of binge episodes may provide powerful motivation for change while also creating psychological barriers to believing that recovery is possible.
Rock bottom experiences often occur during or as a result of binge episodes, as the concentrated nature of problems created during binges can overwhelm normal coping and denial mechanisms. These crisis experiences may provide crucial motivation for seeking treatment and committing to recovery.
Recovery measurement becomes complex for binge drinkers, as extended periods of abstinence between binges may create false confidence while individual binge episodes may seem like complete failures rather than learning experiences. Treatment must help reframe the recovery process in ways that account for binge patterns.
Sponsor relationships and support group participation may require special consideration for binge drinkers, who may feel different from group members with daily drinking patterns and may struggle with shame about the dramatic nature of their drinking episodes.
Prevention and Early Intervention:
Preventing binge drinking episodes often requires identifying and managing triggers before they reach crisis proportions, making early intervention strategies crucial for people with binge drinking patterns.
Trigger management involves identifying personal, emotional, environmental, and social factors that typically precede binge episodes and developing specific strategies for managing these high-risk situations. This may include avoiding certain environments, developing alternative coping strategies for emotional stress, or creating accountability systems during high-risk periods.
Emergency planning becomes crucial for binge drinkers, who need specific strategies for managing crisis situations that typically trigger binges. This may include emergency contact lists, crisis intervention resources, or predetermined action plans for high-risk situations.
Support system development must account for the unique needs of binge drinkers, who may need intensive support during crisis periods but also benefit from accountability during abstinent periods when overconfidence may develop.
Father Martin's identification of binges and benders as a key symptom of alcoholism was crucial because it helped people understand that alcoholism doesn't always manifest as steady daily drinking but can involve patterns of extreme consumption that are equally serious and dangerous. By recognizing binge drinking as a distinct but equally valid form of alcoholism, individuals could seek appropriate treatment for their specific pattern while also understanding that recovery was possible despite the dramatic nature of their drinking episodes. This recognition often provided hope for people who felt their drinking pattern was too severe or chaotic for traditional treatment approaches, while also highlighting the need for specialized treatment strategies that address the unique characteristics of binge drinking patterns.
The Neurophysiology of Alcohol-Related Tremors:
Father Martin's identification of "tremors or shakes" as a symptom of alcoholism revealed one of the most physically visible and medically serious manifestations of alcohol dependency - the point where the body becomes so adapted to alcohol's presence that its absence creates dangerous neurological instability. This symptom represents the transition from psychological dependence to life-threatening physical dependence, where alcohol consumption becomes not just desired but physiologically necessary to prevent potentially fatal withdrawal complications.
Tremors and shakes in alcoholism represent profound changes in the central nervous system's functioning that occur when the brain becomes dependent on alcohol to maintain normal neurochemical balance. Father Martin understood that these physical symptoms were not simply signs of nervousness or anxiety, but evidence of serious neurological adaptation that could become life-threatening without proper medical management.
The development of tremors reflects alcohol's complex effects on neurotransmitter systems, particularly the balance between GABA (gamma-aminobutyric acid), which produces calming effects, and glutamate, which creates excitatory brain activity. Chronic alcohol use suppresses the brain's natural GABA production while enhancing glutamate activity. When alcohol is suddenly removed or reduced, this imbalance creates hyperexcitability in the nervous system that manifests as tremors, agitation, and potentially seizures.
The tremors typically begin as fine movements in the hands that may be barely noticeable during early stages of dependency. However, as physical dependence deepens, the tremors become more pronounced, affecting not just the hands but potentially spreading to involve the entire body. Advanced tremors can be so severe that basic daily activities become impossible without alcohol consumption to provide temporary relief.
The timing of tremors provides crucial information about the severity of physical dependence. Early-stage tremors might only appear after extended periods without alcohol, such as upon waking after a night's sleep. As dependency progresses, tremors may appear within hours of the last drink, eventually requiring almost constant alcohol consumption to prevent their onset.
The intensity of tremors often correlates with the level of physical dependence and can range from mild hand shakiness that others might not notice to violent whole-body trembling that makes speaking, walking, or performing any coordinated movement extremely difficult. Severe tremors represent a medical emergency requiring immediate professional intervention to prevent progression to seizures or delirium tremens.
The Progression to Full-Time Drinking Management:
The concept that "drinking becomes a full-time job" reveals how advanced alcoholism transforms from episodic consumption to continuous management of blood alcohol levels to prevent withdrawal symptoms. This progression represents one of the most psychologically and physically exhausting aspects of late-stage alcoholism, where every waking moment becomes organized around maintaining adequate alcohol levels to function.
The full-time nature of alcohol management begins when the window between drinks becomes critically short due to rapid metabolism and severe physical dependence. The person may need to drink every few hours, including during the night, to prevent withdrawal symptoms from emerging. This creates a schedule more demanding than most employment, requiring constant attention to timing, dosage, and alcohol availability.
Planning becomes obsessively focused on ensuring continuous alcohol access throughout each day. This involves calculating consumption rates, planning purchasing strategies, coordinating alcohol supplies for different locations (home, work, car), and developing backup plans for situations where normal alcohol access might be interrupted. The mental energy devoted to this planning can become all-consuming, leaving little cognitive capacity for other life activities.
The logistics of maintaining continuous alcohol consumption create numerous practical challenges that must be constantly managed. This includes concealing drinking from family and coworkers, managing breath odor and other physical signs of consumption, coordinating bathroom breaks for discrete drinking, and maintaining functional behavior while continuously intoxicated.
Sleep becomes fragmented and problematic as alcohol's effects wear off during the night, often requiring middle-of-the-night drinking to prevent withdrawal symptoms from disrupting sleep. Many people in this stage keep alcohol beside their bed specifically for managing nighttime withdrawal symptoms, turning even sleep into part of the full-time drinking management routine.
Work performance often deteriorates significantly as the demands of managing alcohol consumption compete with job responsibilities. The person may spend work time planning alcohol procurement, take frequent breaks for discrete drinking, or struggle with concentration and productivity due to the constant focus on maintaining optimal blood alcohol levels.
The Need to Return to a "Certain Level" - Baseline Management:
The concept of needing to get back to a "certain level" reveals how advanced alcoholism creates a specific target blood alcohol concentration that feels necessary for normal functioning. This is fundamentally different from drinking for pleasure or social reasons - it represents drinking to achieve a physiological baseline that has become the new definition of normal.
The "certain level" typically develops gradually as tolerance increases and physical dependence deepens. What once felt like mild intoxication eventually becomes the minimum alcohol concentration needed to prevent withdrawal symptoms and function in daily activities. This level becomes as essential as maintaining adequate blood sugar or blood pressure - a physiological necessity rather than a recreational choice.
Identifying and maintaining this level requires sophisticated self-monitoring and adjustment throughout the day. The person becomes acutely aware of subtle changes in how they feel as blood alcohol concentration fluctuates, learning to recognize early signs that alcohol levels are dropping below their functional threshold. This monitoring can become so precise that they can estimate their blood alcohol content based on physical sensations and adjust consumption accordingly.
The maintenance level often differs based on circumstances and requirements. The person may maintain lower levels during work hours while still preventing withdrawal symptoms, then increase to higher levels during evening hours when functional demands are reduced. Weekend levels might be higher than weekday levels, but even during "relaxation" periods, the alcohol consumption is primarily about maintaining physiological stability rather than achieving euphoria.
Panic and anxiety often emerge when circumstances threaten the ability to maintain the necessary level. Running low on alcohol supplies, being in situations where drinking is impossible or monitored, or facing extended periods without access to alcohol can create intense anxiety that goes beyond simple craving - it represents fear of potentially dangerous withdrawal symptoms.
The "certain level" requirement often leads to precise calculation and measurement of alcohol consumption that resembles medical dosing more than recreational drinking. The person may know exactly how much alcohol they need to consume at specific intervals to maintain their functional baseline, treating alcohol like medication required for survival.
Loss of Body Control - The Physical Manifestations:
The loss of body control associated with alcohol tremors extends far beyond simple hand shakiness to encompass a wide range of neurological and motor function impairments that can significantly affect daily functioning and quality of life. These physical symptoms represent the most visible evidence of how alcohol dependency affects the central nervous system and overall bodily function.
Fine motor control deterioration typically begins with difficulty performing precise tasks that require steady hands. Writing becomes shaky and illegible, using utensils becomes challenging, and tasks requiring manual dexterity like buttoning clothes or tying shoes become frustratingly difficult. These impairments often fluctuate based on time since last drink and can be temporarily improved by alcohol consumption.
Gross motor function can also be affected as tremors progress, impacting walking stability, balance, and coordination. The person may develop an unsteady gait, experience difficulty with stairs or uneven surfaces, or find that their overall coordination is compromised. These symptoms can be dangerous, increasing fall risk and accident potential.
Voice tremor often accompanies hand tremors, creating a shaky, unsteady quality to speech that can be embarrassing and may alert others to the presence of alcohol-related problems. The voice may quaver or break, particularly during stressful situations or when alcohol levels are low. This can significantly impact professional interactions and social confidence.
Facial tremors may develop in advanced cases, affecting the muscles around the eyes, mouth, or jaw. These visible facial movements can be particularly distressing because they're difficult to hide and may be the first sign that alerts others to the presence of serious alcohol-related health problems.
Internal tremor sensations can be as distressing as visible shaking, involving feelings of internal vibration, restlessness, or agitation that create constant discomfort even when external tremors aren't visible to others. These internal sensations can be exhausting and anxiety-provoking, contributing to the desperate need for alcohol relief.
The Medical Dangers of Alcohol Tremors:
Tremors represent a serious medical warning sign that indicates the potential for life-threatening withdrawal complications if alcohol consumption is suddenly stopped without proper medical supervision. Father Martin understood that these symptoms required immediate medical attention rather than simply willpower or gradual reduction attempts.
Seizure risk becomes significantly elevated when tremors are present, as both symptoms indicate central nervous system hyperexcitability that can progress to convulsions. Alcohol withdrawal seizures can occur even in people with no previous seizure history and can be fatal if not properly managed in medical settings.
Delirium tremens (DTs) represents the most severe form of alcohol withdrawal and can develop in people experiencing tremors if withdrawal continues without medical intervention. DTs involves confusion, hallucinations, severe agitation, hyperthermia, and cardiovascular instability that can be fatal in 5-15% of cases even with medical treatment.
Cardiovascular complications often accompany severe tremors as the hyperexcited nervous system affects heart rate and blood pressure regulation. This can lead to dangerous elevations in blood pressure, irregular heart rhythms, or cardiovascular collapse that requires immediate medical intervention.
Dehydration and electrolyte imbalances frequently occur alongside tremors as the person may have difficulty maintaining adequate nutrition and hydration due to nausea, vomiting, or preoccupation with alcohol consumption. These imbalances can worsen neurological symptoms and increase the risk of serious complications.
The Psychological Impact of Visible Tremors:
The development of visible tremors often represents a psychological crisis point where the person can no longer deny the severity of their alcohol dependency. Unlike many other symptoms of alcoholism that can be hidden or rationalized, tremors provide undeniable physical evidence of serious health problems that become increasingly difficult to explain away.
Shame and embarrassment about tremors can drive increased social isolation as the person becomes aware that their physical symptoms are visible to others and may invite questions or concern. Simple activities like signing documents, handling money, or eating in public can become sources of anxiety and humiliation.
Professional consequences often arise when tremors become visible in work settings, as employers, colleagues, or clients may notice the shaking and question the person's health or fitness for duty. This can lead to forced medical evaluations, disciplinary actions, or job loss that create additional stress and motivation for continued drinking.
Family relationships are often profoundly affected when tremors become apparent, as loved ones may finally have visible evidence of the severity of alcohol-related health problems. This can lead to increased family pressure for treatment, interventions, or ultimatums that create additional stress while also potentially providing motivation for change.
The unpredictability of tremor severity can create anxiety about public appearances and social interactions. Not knowing how severe tremors will be at any given time makes planning social or professional activities extremely difficult and can lead to increased isolation and avoidance of commitments.
The Cycle of Tremor Relief and Dependency Deepening:
The temporary relief that alcohol provides for tremors creates a vicious cycle that deepens physical dependency while providing immediate evidence of alcohol's "medicinal" properties. This cycle becomes self-reinforcing and increasingly difficult to break without professional intervention.
Immediate relief from alcohol consumption provides powerful reinforcement for continued drinking, as the person experiences dramatic and rapid improvement in tremor severity within minutes of consuming alcohol. This immediate cause-and-effect relationship makes alcohol feel like necessary medicine rather than the cause of the underlying problem.
Tolerance to the anti-tremor effects of alcohol develops over time, requiring increasing amounts of alcohol to achieve the same level of tremor control. This drives consumption levels higher while making the tremors more severe during periods when alcohol levels drop, creating an escalating cycle of dependency.
The fear of tremor onset often leads to preemptive drinking to prevent symptoms rather than waiting for them to appear. This preventive approach typically results in higher overall consumption levels and shorter intervals between drinks as the person attempts to stay ahead of withdrawal symptoms.
Rebound tremors often occur as alcohol effects wear off, frequently more severe than the baseline tremors that prompted drinking. This rebound effect creates the need for increasingly frequent alcohol consumption to prevent progressively worse withdrawal symptoms.
Medical Management and Treatment Considerations:
Treating tremors associated with alcoholism requires specialized medical approaches that address both the immediate symptoms and the underlying physical dependency. Father Martin emphasized that these symptoms required professional medical intervention rather than self-treatment or gradual reduction attempts.
Medical detoxification typically requires inpatient monitoring when significant tremors are present, as the risk of seizures, delirium tremens, and other life-threatening complications necessitates 24-hour medical supervision and immediate access to emergency interventions.
Benzodiazepine medications are commonly used during medical detoxification to manage tremors and prevent seizures by providing temporary GABA system support while the brain readjusts to functioning without alcohol. These medications require careful dosing and monitoring to prevent complications while providing adequate symptom control.
Nutritional support becomes crucial during detoxification as alcohol-related malnutrition, particularly thiamine (vitamin B1) deficiency, can worsen neurological symptoms and increase the risk of permanent brain damage. IV vitamin supplementation may be necessary during acute withdrawal management.
Gradual dose reduction protocols are sometimes used in outpatient settings for people with less severe tremors, but this approach requires close medical supervision and careful monitoring for signs of withdrawal escalation that might require immediate hospitalization.
Long-term Neurological Recovery:
Recovery from alcohol-related tremors can be variable, with some people experiencing complete resolution while others may have persistent neurological effects even after sustained abstinence. Understanding the potential for recovery can provide hope while also emphasizing the importance of early intervention.
Neuroplasticity allows for significant brain healing during sustained abstinence, with many people experiencing gradual improvement in tremor severity over weeks or months of sobriety. However, the extent of recovery often depends on the duration and severity of alcohol use before treatment.
Essential tremor may persist in some people even after successful alcohol treatment, representing either pre-existing neurological conditions that were masked by alcohol use or permanent neurological damage from chronic alcohol exposure. These persistent tremors may require ongoing medical management.
Stress sensitivity often remains elevated even after tremors resolve, with many people in recovery finding that their hands shake during stress, fatigue, or emotional situations even when alcohol hasn't been consumed for extended periods. Learning stress management techniques becomes important for preventing these situational tremors.
The Family Perspective on Tremors:
Family members often experience tremors as particularly frightening symptoms because they provide visible evidence of serious health problems that can no longer be denied or minimized. This visibility can be both helpful for motivating treatment and traumatic for loved ones who witness the physical deterioration.
Caregiver burden increases significantly when tremors affect the person's ability to perform basic daily activities independently. Family members may need to assist with eating, writing, dressing, or other activities that tremors make difficult, creating additional stress and time demands.
Safety concerns become prominent when tremors affect driving ability, cooking safety, or other activities that could be dangerous if motor control is compromised. Family members often struggle with how much independence to allow while also protecting their loved one and others from potential harm.
Children in families affected by alcohol-related tremors may be particularly frightened by seeing a parent shake uncontrollably, especially if they don't understand the medical nature of the symptoms. Age-appropriate education about the medical aspects of addiction can help reduce fear while also providing understanding about the need for treatment.
Workplace Implications and Accommodations:
Alcohol-related tremors can have significant implications for employment, particularly in jobs requiring fine motor skills, public interaction, or safety-sensitive activities. Understanding legal rights and accommodation options becomes important for maintaining employment during treatment.
Americans with Disabilities Act (ADA) protections may apply to people with alcohol-related tremors who are seeking treatment, requiring employers to provide reasonable accommodations that allow continued employment while addressing health problems. However, this protection typically requires active participation in treatment programs.
Safety-sensitive positions may require temporary or permanent job modifications when tremors affect the ability to perform essential job functions safely. This might include reassignment to different duties, modified schedules to accommodate treatment, or extended leave for intensive treatment programs.
Professional licensing issues may arise for people in licensed professions when alcohol-related tremors become apparent or interfere with professional duties. Many licensing boards have specific protocols for addressing substance use disorders that may include monitoring programs, treatment requirements, or practice restrictions.
Treatment Integration and Recovery Planning:
Addressing tremors as part of comprehensive addiction treatment requires integrating medical management with psychological and social interventions that address the underlying alcohol dependency. The dramatic nature of tremor symptoms often provides powerful motivation for treatment engagement.
Motivational enhancement around health consequences can be particularly effective when tremors are present, as these symptoms provide clear evidence of serious health problems that may motivate commitment to treatment and lifestyle change.
Relapse prevention planning must address the powerful reinforcement that alcohol provides for tremor relief, helping people develop alternative strategies for managing anxiety and stress that might trigger drinking episodes.
Family therapy often needs to address the trauma and fear that family members experience when witnessing alcohol-related tremors, while also providing education about the medical nature of these symptoms and appropriate responses during crisis situations.
The Spiritual and Existential Dimensions:
For many people, the development of tremors represents a spiritual crisis where they must confront their mortality and the serious consequences of their alcohol use. This crisis can provide motivation for fundamental life changes that extend beyond simply stopping drinking.
Surrender and acceptance often become necessary psychological processes when tremors make it impossible to maintain the illusion of control over alcohol use. The visible evidence of physical dependency can break through denial and create openness to accepting help and treatment.
Meaning-making around the tremor experience can be important for recovery, as people work to understand how their alcohol use progressed to such serious health consequences and what changes are necessary to prevent further deterioration.
Hope for recovery can be fostered by understanding that tremors often improve significantly with sustained abstinence and appropriate medical care, providing motivation for the difficult work of early recovery when withdrawal symptoms may be severe.
Father Martin's identification of tremors and shakes as a cardinal symptom of alcoholism was crucial because it helped people understand that their physical symptoms represented serious medical complications requiring immediate attention rather than simply nervous habits or stress reactions. By recognizing tremors as evidence of life-threatening physical dependency, individuals could seek appropriate medical treatment while also understanding that recovery was possible with proper medical support and comprehensive addiction treatment. This recognition often provided the motivation necessary for people to overcome denial and seek the intensive treatment required for safely managing alcohol withdrawal and establishing sustained recovery.
The Psychology of Supply Protection:
Father Joseph Martin's identification of "protecting the supply" as a symptom of alcoholism revealed one of the most psychologically revealing and practically devastating aspects of advanced alcohol dependency - the systematic reorganization of life priorities around ensuring continuous access to alcohol. This symptom demonstrates how alcoholism progressively hijacks the brain's survival instincts, transforming alcohol from a recreational substance into something perceived as essential for survival, worthy of protection at the expense of all other life responsibilities and relationships.
The drive to protect alcohol supplies represents a fundamental shift in the brain's priority system where alcohol access becomes more important than food, shelter, relationships, employment, or other basic human needs. Father Martin understood that this wasn't simply poor decision-making or lack of willpower, but rather evidence of how addiction rewires the brain's reward and survival circuits to prioritize the addictive substance above all other considerations.
The protection mentality develops gradually as the person learns from experience that running out of alcohol creates intense physical and psychological distress that feels unbearable. This learning process creates powerful associations between alcohol shortage and survival threat, triggering primitive hoarding and protection behaviors that are typically reserved for truly essential resources like food or water during times of scarcity.
The sophistication of supply protection strategies often increases over time, evolving from simple backup purchases to complex systems involving multiple stash locations, various suppliers, and elaborate concealment methods. The mental energy and planning devoted to supply protection can become all-consuming, demonstrating how alcohol has assumed central importance in the person's cognitive and emotional life.
Security thinking begins to dominate decision-making processes as the person constantly assesses potential threats to their alcohol supply. This might include family members who might discover and dispose of hidden alcohol, financial limitations that might restrict purchasing ability, or social situations that might interfere with normal consumption patterns. The constant vigilance required for supply protection creates chronic stress and anxiety that paradoxically drives increased alcohol consumption.
Contingency planning becomes elaborate and automatic as the person develops multiple backup strategies for ensuring alcohol access under various circumstances. This planning might include identifying 24-hour liquor stores, maintaining multiple credit cards for alcohol purchases, or establishing relationships with different suppliers to ensure availability even if primary sources are compromised.
The Prioritization Shift - Other Things Become Less Important:
The gradual devaluation of previously important life priorities represents one of the most tragic aspects of alcoholism's progression. Activities, relationships, and responsibilities that once provided meaning and satisfaction become obstacles to alcohol consumption rather than sources of fulfillment and purpose.
Career advancement often becomes secondary to maintaining alcohol access and consumption routines. Professional development opportunities might be declined if they interfere with drinking schedules, networking events might be avoided if alcohol access is uncertain, and work performance might deteriorate as energy and attention become focused on alcohol-related concerns rather than professional excellence.
Family relationships frequently suffer as alcohol-related priorities take precedence over family needs and obligations. Children's activities might be missed if they conflict with drinking routines, family vacations might be planned around alcohol availability rather than family interests, and intimate relationships might be neglected as emotional energy becomes consumed with alcohol-related concerns.
Personal health and self-care often deteriorate as resources and attention previously devoted to exercise, nutrition, medical care, and personal hygiene are redirected toward alcohol procurement and consumption. The irony that alcohol dependency drives neglect of the very health that alcohol is damaging often becomes apparent only in retrospect.
Creative pursuits and hobbies that once provided satisfaction and identity may be abandoned if they interfere with drinking routines or require sustained concentration that alcohol consumption impairs. Musical instruments gather dust, art supplies remain unused, and books go unread as alcohol becomes the primary source of entertainment and stimulation.
Social activities become filtered through alcohol availability rather than personal interest or relationship value. Invitations to alcohol-free events might be declined, friendships with non-drinkers might be neglected, and social planning becomes organized around alcohol access rather than meaningful connection or shared interests.
Financial Prioritization - Past Due Bills and Obligations:
The financial prioritization of alcohol over essential expenses represents one of the most visible and practically devastating consequences of supply protection behavior. As alcohol assumes emergency-level importance in the person's psychological hierarchy, normal financial planning and responsibility become secondary considerations.
Essential bill payment often becomes erratic as available money is redirected toward alcohol purchases. Rent or mortgage payments might be delayed, utility services might be disconnected, and insurance policies might lapse as alcohol purchases take precedence over these seemingly less urgent expenses. The immediate relief provided by alcohol consumption often outweighs the delayed consequences of financial neglect.
Credit card debt frequently accumulates rapidly as alcohol purchases exceed available income. The person might use credit cards specifically for alcohol purchases to preserve cash for other expenses, or might use cash advances to maintain alcohol supplies when other payment methods are unavailable. The high interest rates and fees associated with credit card debt compound the financial damage over time.
Emergency fund depletion commonly occurs as savings accounts are systematically emptied to maintain alcohol supplies during financial stress periods. Money set aside for emergencies, vacations, or major purchases becomes viewed as available alcohol funding, eliminating financial security and creating vulnerability to life crises.
Borrowing patterns often develop as the person seeks additional funding sources for alcohol purchases when normal income proves insufficient. This might include borrowing from family members, friends, employers, or financial institutions, often under false pretenses about the intended use of borrowed money.
The mathematical irrationality of alcohol prioritization often becomes apparent when examining actual spending patterns. A person might spend hundreds of dollars monthly on alcohol while allowing relatively small bills to go unpaid, demonstrating how addiction distorts normal cost-benefit analysis and decision-making processes.
Long-term Financial Consequences:
The protection of alcohol supplies at the expense of financial obligations creates cascading consequences that can take years to resolve even after achieving sobriety. The financial damage often continues long after alcohol consumption stops, affecting credit ratings, living situations, and financial stability throughout recovery.
Credit score destruction occurs when bills consistently go unpaid in favor of alcohol purchases. Poor credit ratings can affect employment opportunities, housing options, insurance rates, and loan availability for years after recovery begins. The financial consequences of alcohol prioritization often outlast the addiction itself.
Asset liquidation frequently occurs as the person sells valuable possessions to maintain alcohol supplies when other funding sources are exhausted. Cars, jewelry, electronics, collectibles, and other valuable items might be sold at below-market prices to generate quick cash for alcohol purchases, representing permanent loss of accumulated wealth.
Bankruptcy filings may become necessary when alcohol-related financial damage becomes overwhelming and unmanageable. The legal and financial consequences of bankruptcy can affect financial opportunities for seven to ten years, creating long-term barriers to financial recovery and stability.
Employment consequences often result from financial irresponsibility related to alcohol prioritization. Garnished wages, poor credit checks, or financial stress-related performance problems can affect career advancement and employment stability, creating additional financial pressure and stress.
Strategic Supply Management - Stocking Up for Long Weekends:
The practice of stocking up for extended periods reveals the sophisticated planning and anticipatory anxiety that characterizes advanced alcoholism. This behavior demonstrates how the person has learned to think strategically about alcohol access, treating it like a essential commodity that must be carefully managed to prevent shortage crises.
Holiday and weekend preparation often becomes elaborate projects involving careful calculation of consumption rates, availability of suppliers during closure periods, and contingency planning for unexpected consumption increases. The person might purchase significantly more alcohol than normal to ensure adequate supplies during periods when stores are closed or access might be limited.
Event planning increasingly revolves around alcohol logistics rather than social or recreational considerations. Family gatherings, vacations, business trips, or other events are assessed primarily in terms of alcohol access and consumption opportunities, with secondary consideration given to social, professional, or personal aspects of these occasions.
Inventory management systems often develop as the person maintains careful awareness of current alcohol supplies, consumption rates, and projected needs. This might involve mental or written tracking of alcohol quantities, rotation of stored supplies to prevent spoilage, and regular assessment of storage capacity and concealment effectiveness.
Emergency reserves become standard practice as the person maintains backup alcohol supplies for unexpected situations that might threaten normal consumption routines. These reserves might be hidden in various locations to ensure access even if primary supplies are discovered or compromised, demonstrating the paranoid thinking that often accompanies addiction.
The anxiety associated with potential shortages can become overwhelming, driving excessive purchasing that creates financial strain while also providing psychological relief about alcohol security. The fear of running out often motivates purchasing decisions that exceed actual consumption needs, creating waste and additional financial burden.
The Geography of Supply Protection:
Supply protection often involves complex geographical strategies designed to ensure alcohol access across different locations and situations where the person spends time. This geographic distribution reflects both the mobility of modern life and the persistent need for alcohol access regardless of location.
Multiple stash locations become common as the person hides alcohol supplies in various places to ensure access when needed. This might include alcohol hidden at home, in cars, at workplaces, or even in outdoor locations that provide secure but accessible storage. The complexity of these distribution systems demonstrates the planning and energy devoted to supply protection.
Transportation considerations often influence alcohol purchasing and storage decisions as the person ensures that alcohol can be safely and discretely transported between locations without detection or legal problems. This might involve specific containers, timing strategies, or route planning to minimize risk while maintaining access.
Work-related storage can become particularly complex as the person attempts to maintain alcohol access during work hours without detection by supervisors or colleagues. Office stashes, car supplies, or nearby commercial storage might be used to ensure access during the workday while avoiding obvious workplace drinking.
Travel planning increasingly revolves around alcohol access and transportation logistics rather than destination attractions or business purposes. Hotel selection might be based on alcohol policies or nearby purchasing options, flight selection might consider alcohol service or carry-on restrictions, and itinerary planning might include time for alcohol procurement at destinations.
Social Manipulation for Supply Protection:
Advanced alcoholism often involves sophisticated social manipulation designed to protect alcohol supplies and access while maintaining the appearance of normal social functioning. These manipulation strategies can damage relationships while serving the primary goal of supply protection.
Family manipulation might involve elaborate deception about alcohol quantities, consumption patterns, or purchasing frequency. The person might hide purchases from family members, lie about consumption levels, or manipulate family schedules to create opportunities for secretive alcohol procurement and consumption.
Financial deception often extends to elaborate explanations for alcohol-related expenses or mysterious disappearances of money allocated for other purposes. Credit card statements might be hidden, cash purchases might be made to avoid paper trails, or alternative explanations might be created for alcohol-related financial irregularities.
Social pressure tactics can be used to ensure alcohol availability in social situations where hosts might not provide adequate supplies. This might involve bringing alcohol to events under various pretenses, pressuring hosts to provide specific types or quantities of alcohol, or manipulating event planning to ensure alcohol centrality.
Workplace manipulation might involve deceptive explanations for alcohol-related absences, performance problems, or behavioral changes. Elaborate justifications might be created for lunch hour absences, afternoon performance declines, or other alcohol-related workplace issues that threaten employment stability.
The Technology of Modern Supply Protection:
Modern technology has created new opportunities and challenges for alcohol supply protection, with smartphones, delivery services, and digital payment systems providing both enhanced access and potential detection risks.
Delivery services can provide discrete alcohol access without the need for public purchasing that might be observed by family members, friends, or colleagues. However, delivery records and payment trails can create digital evidence of consumption patterns that might be discovered later.
Digital payment systems create detailed records of alcohol purchases that can reveal consumption patterns and frequencies to family members who share accounts or have access to financial records. This has led to increased use of cash purchases or separate payment accounts specifically for alcohol procurement.
Location tracking through smartphones can create complications for secretive alcohol purchasing as family members might question unexplained stops at liquor stores or bars. This has led to more sophisticated planning about when and where alcohol purchases occur to avoid creating suspicious location patterns.
Online research about alcohol availability, prices, and access has become common as people research the most efficient and discrete methods for obtaining alcohol in various locations and circumstances. This research effort demonstrates the priority that alcohol access has assumed in daily planning and decision-making.
The Impact on Living Situations:
Supply protection often influences housing decisions and living arrangements as the person prioritizes alcohol access and storage over other considerations that might normally influence residential choices.
Housing selection might be influenced by proximity to liquor stores, privacy for alcohol storage and consumption, or ability to receive alcohol deliveries without detection. Neighborhoods, apartment features, or house characteristics might be evaluated primarily in terms of their compatibility with alcohol use rather than other lifestyle preferences.
Roommate and family negotiations often revolve around alcohol policies, storage arrangements, and consumption boundaries rather than normal shared living considerations. The person might avoid living situations where alcohol use would be monitored or restricted, even if these situations would otherwise be preferable.
Storage solutions become increasingly sophisticated as the person develops systems for hiding and protecting alcohol supplies within shared living spaces. This might involve specialized furniture, concealment devices, or distribution strategies that prevent detection while ensuring easy access when needed.
Privacy protection becomes paramount as the person works to prevent family members, roommates, or visitors from discovering alcohol supplies or consumption patterns. This might involve elaborate scheduling of alcohol-related activities, noise management during consumption periods, or deception about normal daily routines.
The Psychological Burden of Supply Protection:
The constant vigilance required for effective supply protection creates significant psychological stress that often goes unrecognized as a factor in the overall suffering associated with alcoholism. The mental energy devoted to these protection activities can be exhausting and anxiety-provoking.
Paranoid thinking often develops as the person becomes hypervigilant about threats to their alcohol supply. Family members, friends, employers, or authority figures might be viewed with suspicion as potential threats to alcohol access, creating interpersonal tension and isolation that compounds other alcohol-related social problems.
Cognitive load increases significantly as the person maintains awareness of alcohol inventory levels, consumption rates, supplier availability, financial resources for purchasing, and potential threats to access. This constant mental processing can interfere with concentration, memory, and decision-making in other life areas.
Anticipatory anxiety about potential shortages can become overwhelming, creating persistent worry about future alcohol access even when current supplies are adequate. This anxiety often drives excessive purchasing and hoarding behaviors that create financial strain while providing temporary psychological relief.
The exhaustion associated with managing complex supply protection systems can contribute to the overall deterioration in functioning that characterizes advanced alcoholism. The energy required for these activities often exceeds the energy available for maintaining normal life responsibilities and relationships.
Recovery Challenges Related to Supply Protection:
Addressing supply protection behaviors in recovery requires understanding how deeply these patterns have become embedded in daily routines, financial planning, and psychological functioning. The systematic dismantling of protection systems often represents a significant component of early recovery work.
Financial recovery planning must address the debt and financial damage created by alcohol prioritization while also establishing new systems for managing money without the compulsive drive to ensure alcohol access. This often requires professional financial counseling and systematic debt management strategies.
Trust rebuilding with family members often focuses heavily on financial transparency and responsibility demonstration, as family members may have been particularly hurt by the financial consequences of alcohol prioritization. Shared financial planning and accountability systems often become necessary components of relationship repair.
Anxiety management becomes crucial as the person learns to live without the psychological security provided by protected alcohol supplies. Learning alternative coping strategies for anxiety and uncertainty often requires professional counseling and medication management during early recovery.
Routine restructuring involves developing new daily and weekly routines that don't revolve around alcohol procurement, storage, and consumption. This often requires professional help to develop meaningful alternative activities and priorities that can provide structure and purpose in recovery.
The Family Perspective on Supply Protection:
Family members often experience supply protection behaviors as particularly hurtful and confusing because they provide clear evidence that alcohol has become more important than family welfare, financial security, and shared responsibilities. This prioritization can feel like personal rejection and betrayal.
Financial stress on families can be devastating when alcohol purchases take precedence over essential family expenses. Spouses might struggle to maintain household functions while trying to protect family financial security from alcohol-related spending. Children might go without necessities while alcohol supplies are maintained.
Trust erosion often centers around financial deception and the discovery of hidden alcohol supplies or purchases. Family members may feel betrayed not just by the alcohol use itself, but by the elaborate deception and manipulation required to protect supplies and access.
Safety concerns may arise when family members discover that essential expenses like insurance, utilities, or car maintenance have been neglected in favor of alcohol purchases. The potential consequences of these neglected obligations can create anxiety and resentment among family members.
The detective work that family members often feel compelled to do to understand financial irregularities or discover hidden supplies can create an adversarial dynamic that damages relationships and creates additional stress for everyone involved.
Professional and Legal Consequences:
Supply protection behaviors often create professional and legal consequences that extend far beyond the immediate alcohol use, affecting career prospects and legal standing in ways that can persist long after recovery begins.
Employment consequences may result from financial irresponsibility, theft of time or resources for alcohol procurement, or performance problems related to supply protection stress. Employers may discover financial irregularities, time abuse, or other alcohol-related workplace violations that result in disciplinary action or termination.
Legal problems can arise from financial crimes committed to maintain alcohol supplies, such as theft, embezzlement, or fraud. The desperation to protect access and funding for alcohol can drive criminal behavior that creates legal consequences lasting far beyond the addiction itself.
Professional licensing issues may develop when supply protection behaviors affect job performance or professional responsibilities. Licensed professionals may face ethics violations, practice restrictions, or license revocation related to alcohol-related financial or performance problems.
Civil consequences might include lawsuits, garnishments, or asset seizure related to unpaid obligations that were neglected in favor of alcohol prioritization. These legal actions can create additional financial and emotional stress during recovery.
Father Martin's identification of supply protection as a cardinal symptom of alcoholism was crucial because it helped people understand that their financial irresponsibility and priority distortions were symptoms of a disease rather than moral failings or character defects. By recognizing how addiction systematically rewires the brain's priority system to favor alcohol over all other considerations, individuals could begin to address these behaviors through comprehensive treatment that addressed both the addiction and its consequences. This understanding often provided relief from shame while also highlighting the need for systematic financial and life reconstruction as part of the recovery process.
The recognition that supply protection behaviors represent survival-level brain responses rather than conscious choices helped families understand that their loved one's apparent selfishness and irresponsibility were symptoms of a medical condition rather than evidence that they no longer cared about family welfare. This understanding, while painful, often provided the framework necessary for both seeking appropriate treatment and beginning the long process of financial and relationship repair that recovery requires.
The Neurochemical Foundation of Alcohol-Related Anxiety:
Father Martin's identification of "nameless fears and anxiety" as a symptom of alcoholism revealed one of the most psychologically torturous and least understood aspects of alcohol dependency - the development of pervasive, irrational fears and anxieties that seem to have no logical basis but create overwhelming distress that drives continued alcohol use. This symptom exposes how alcoholism fundamentally alters brain chemistry and psychological functioning, creating a state of chronic hypervigilance and terror that can persist even during periods of sobriety.
The development of nameless fears and anxiety in alcoholism reflects profound changes in the brain's neurochemical systems that regulate mood, stress response, and threat perception. Father Martin understood that these weren't simply psychological weaknesses or character defects, but rather evidence of how chronic alcohol use systematically disrupts the brain's natural anxiety regulation mechanisms.
Alcohol's effects on the GABA (gamma-aminobutyric acid) system create a neurochemical dependency where the brain reduces its natural production of calming neurotransmitters in response to alcohol's artificial GABA enhancement. When alcohol levels drop, the brain is left with insufficient natural anxiety regulation, creating a state of hyperarousal and fear that feels overwhelming and inexplicable.
The glutamate system, which creates excitatory brain activity, becomes hyperactive during alcohol withdrawal as the brain attempts to compensate for alcohol's depressant effects. This hyperexcitation creates racing thoughts, agitation, and a heightened startle response that makes normal environmental stimuli feel threatening and overwhelming.
Norepinephrine and dopamine systems, which regulate mood, motivation, and stress response, also become dysregulated through chronic alcohol use. This dysregulation can create symptoms resembling panic disorder, generalized anxiety disorder, and even paranoid thinking patterns that persist between drinking episodes and often worsen over time.
The amygdala, the brain's fear center, becomes hyperactive in people with alcoholism, creating an exaggerated threat response to situations that wouldn't normally provoke anxiety. This hyperactivity can persist for months or even years after alcohol cessation, creating persistent vulnerability to anxiety and fear responses that seem disproportionate to actual circumstances.
The "Nameless" Quality of Alcohol-Related Fears:
The description of fears as "nameless" captures one of the most distressing aspects of alcohol-related anxiety - the sense that terror and dread are present without any identifiable cause or rational explanation. This quality distinguishes alcohol-related anxiety from normal worry or concern about specific life circumstances.
Existential dread often characterizes these nameless fears, involving a profound sense that something terrible is about to happen without any ability to identify what that might be. This vague but overwhelming sense of impending doom can create constant vigilance and anxiety that exhausts mental and emotional resources while providing no clear target for problem-solving or coping strategies.
The inability to identify the source of fear creates additional anxiety about the anxiety itself, leading to a cycle where fear of fear becomes as problematic as the original anxiety symptoms. The person may worry about when the next anxiety episode will occur, how severe it will be, or whether they're losing their sanity, creating secondary fears that compound the original problem.
Somatic anxiety often manifests without clear psychological content, involving physical symptoms like racing heart, shortness of breath, sweating, or trembling that occur without any conscious awareness of fearful thoughts or specific triggers. These physical symptoms can be terrifying because they seem to come from nowhere and suggest serious medical problems.
The primitive nature of these fears often bypasses rational thinking entirely, activating survival-level responses that feel life-threatening even when no actual danger is present. This primitive activation makes it impossible to "think your way out" of the anxiety using logic or reasoning, leaving the person feeling helpless against overwhelming terror.
Fear of People, Places, and Things - Agoraphobic Responses:
The development of fears related to people, places, and things represents a progressive restriction of the person's world as alcohol-related anxiety makes normal environments and interactions feel threatening and dangerous. This symptom often leads to increasing isolation and avoidance that compounds other problems associated with alcoholism.
Social anxiety often becomes overwhelming as alcohol withdrawal and brain chemistry changes make normal human interaction feel threatening and overwhelming. Simple conversations can trigger intense anxiety, making workplace interactions, family gatherings, or casual social encounters feel dangerous and to be avoided. The irony that alcohol often initially served as a social lubricant makes this social anxiety particularly cruel and isolating.
Public places frequently become sources of intense anxiety as the hypervigilant brain interprets normal environmental stimuli as threatening. Grocery stores, shopping malls, restaurants, or other public venues can trigger panic attacks or overwhelming anxiety that drives immediate escape and future avoidance. The unpredictability of when these episodes might occur creates anticipatory anxiety about leaving home.
Specific locations associated with drinking or alcohol-related incidents often become trigger sites that provoke intense anxiety and fear. Bars, restaurants, liquor stores, or even neighborhoods where drinking occurred can create overwhelming anxiety that seems disproportionate but reflects the brain's learned associations between these locations and alcohol-related distress.
Work environments may become sources of intense anxiety as alcohol-related changes in confidence, concentration, and stress tolerance make normal job responsibilities feel overwhelming and threatening. Performance anxiety, fear of discovery of alcohol-related problems, or simple difficulty concentrating can make workplace attendance feel impossible.
Medical settings often trigger intense anxiety in people with alcohol-related health problems, as doctor's offices or hospitals become associated with shame, discovery, or confrontation about alcohol use. This medical anxiety can prevent important healthcare that might address alcohol-related health problems, creating additional risks and complications.
The progressive nature of place-based fears often leads to an increasingly constricted world where fewer and fewer environments feel safe and manageable. This constriction can eventually lead to agoraphobic patterns where leaving home becomes extremely difficult or impossible without alcohol to manage the anxiety.
Paranoid Thinking Patterns:
The development of paranoid thoughts in alcoholism reflects how alcohol-related brain changes can distort perception and reasoning, creating beliefs that others are watching, judging, or plotting against the person. These paranoid thoughts often have enough connection to reality to seem plausible while being exaggerated far beyond actual circumstances.
Surveillance paranoia commonly involves the belief that others are constantly observing and judging alcohol consumption patterns, behavior, or appearance. The person might believe that store clerks are tracking their alcohol purchases, that coworkers are monitoring their performance for signs of drinking, or that family members are constantly watching for evidence of alcohol use. While some observation may actually be occurring, the paranoid thinking greatly exaggerates the extent and malicious intent of this attention.
Conspiracy thinking can develop where the person believes that multiple people are coordinating efforts to control, punish, or expose their alcohol use. Family members, employers, healthcare providers, or legal authorities might be viewed as working together in elaborate schemes to trap or harm the person. These beliefs often contain kernels of truth - people may indeed be concerned and discussing the person's alcohol use - but the paranoid interpretation vastly overstates the coordination and malicious intent involved.
Persecution beliefs frequently involve the conviction that others are actively trying to harm, embarrass, or sabotage the person because of their alcohol use or other perceived failings. Employers might be viewed as looking for excuses to fire them, family members might be seen as plotting intervention or divorce, or friends might be suspected of spreading gossip or trying to damage relationships.
Mind reading paranoia involves the belief that others can somehow detect alcohol use, thoughts, or intentions through supernatural or highly developed observational skills. The person might believe that others can smell alcohol on them when none is present, that their thoughts are visible to others, or that subtle behavioral changes reveal their alcohol use even when they believe they're concealing it effectively.
The self-fulfilling nature of paranoid thinking often creates the very problems the person fears, as their defensive, suspicious behavior alienates others and creates the rejection and conflict they were afraid of experiencing. This confirmation of fears reinforces the paranoid thinking and creates cycles of increasing isolation and suspicion.
Racing Thoughts and Obsessive Planning:
The phenomenon of racing thoughts about alcohol use reveals how addiction colonizes mental space, creating obsessive preoccupation with procurement, consumption, and protection of alcohol supplies that can consume enormous amounts of mental energy and attention throughout each day.
Procurement planning often becomes elaborate and time-consuming, involving detailed consideration of when, where, and how to obtain alcohol while avoiding detection or interference. The person might spend hours mentally reviewing store locations, optimal purchasing times, payment methods, and concealment strategies. This planning often occurs continuously throughout the day, interfering with concentration on work, relationships, or other activities.
Consumption scheduling frequently involves complex calculations about optimal drinking times, quantities, and spacing to achieve desired effects while avoiding negative consequences. The person might mentally rehearse drinking scenarios, calculate blood alcohol levels, plan eating schedules to optimize absorption, or strategize about timing consumption around work, family, or social obligations.
Concealment strategies occupy significant mental resources as the person continuously plans how to hide alcohol use from family members, employers, healthcare providers, or others who might interfere with their drinking. This might involve elaborate schemes for disposing of evidence, explaining absences or behavior changes, or maintaining appearance of sobriety during important interactions.
Risk assessment becomes constant and exhausting as the person continuously evaluates potential threats to their alcohol supply, consumption opportunities, or concealment efforts. Every interaction, obligation, or change in routine is analyzed for its potential impact on drinking plans, creating a state of hypervigilance that interferes with normal mental functioning.
Contingency planning for various scenarios that might interfere with normal alcohol consumption patterns can become incredibly detailed and elaborate. The person might develop backup plans for holidays when stores are closed, strategies for maintaining consumption during travel, or emergency protocols for situations where normal drinking routines are disrupted.
The Cycle of Anxiety and Alcohol Use:
The relationship between anxiety and alcohol use in alcoholism creates a vicious cycle where anxiety drives drinking, drinking temporarily relieves anxiety, but alcohol use ultimately worsens anxiety symptoms, creating increased need for alcohol to manage the intensified anxiety symptoms.
Alcohol as anxiety medication initially provides genuine relief from overwhelming fear and anxiety symptoms, creating powerful learning that alcohol is effective for managing psychological distress. This relief is real and immediate, making alcohol feel like necessary medicine rather than a recreational drug or the cause of underlying problems.
Tolerance to alcohol's anxiety-relieving effects develops over time, requiring increasing amounts of alcohol to achieve the same level of anxiety relief. This tolerance often develops faster than tolerance to alcohol's intoxicating effects, meaning that dangerous levels of consumption may be required to manage anxiety symptoms effectively.
Rebound anxiety typically occurs as alcohol effects wear off, often creating anxiety levels that are worse than the original symptoms that prompted drinking. This rebound effect drives increasingly frequent alcohol consumption as the person attempts to prevent the return of overwhelming anxiety symptoms.
Withdrawal anxiety can become severe enough to create medical emergencies, particularly when physical dependence has developed and alcohol cessation triggers potentially life-threatening withdrawal symptoms including panic attacks, seizures, or delirium tremens.
The anticipatory anxiety about future anxiety episodes often becomes as problematic as the original anxiety symptoms, creating persistent worry about when the next anxiety attack might occur and whether alcohol will be available to manage it when needed.
Physical Manifestations of Alcohol-Related Anxiety:
The anxiety associated with alcoholism often involves dramatic physical symptoms that can be terrifying and confusing, particularly when they occur without obvious psychological triggers or during periods when the person believes they should feel calm.
Panic attack symptoms including racing heart, shortness of breath, sweating, trembling, nausea, and feelings of impending doom can occur unpredictably and feel life-threatening. These physical symptoms often drive emergency room visits where medical evaluations reveal no cardiac or other physical problems, leading to confusion and frustration about the cause of symptoms.
Insomnia and sleep disturbances become common as alcohol-related anxiety interferes with the ability to fall asleep or stay asleep without alcohol assistance. The person might experience racing thoughts, physical restlessness, or panic symptoms when trying to sleep, creating dependence on alcohol for sleep that worsens overall sleep quality and anxiety levels.
Digestive problems including nausea, stomach pain, diarrhea, or loss of appetite often accompany alcohol-related anxiety, creating additional physical distress that can be misinterpreted as medical problems rather than anxiety symptoms. These gastrointestinal symptoms can be severe enough to interfere with nutrition and overall health.
Muscle tension and pain frequently result from chronic anxiety states, creating headaches, neck pain, back pain, or overall body aches that seem to have no physical cause. This tension can be exhausting and create additional anxiety about potential medical problems.
Hypervigilance and exaggerated startle responses make normal environmental sounds, movements, or changes feel threatening and overwhelming. The person might jump at normal noises, feel constantly "on edge," or experience physical exhaustion from maintaining high levels of alertness throughout the day.
The Impact on Daily Functioning:
Nameless fears and anxiety can severely impair daily functioning, making normal activities feel overwhelming and dangerous while requiring enormous amounts of mental and emotional energy to manage basic life responsibilities.
Work performance often deteriorates significantly as anxiety interferes with concentration, decision-making, and interpersonal functioning. The person might have difficulty completing tasks, participating in meetings, or maintaining professional relationships due to overwhelming anxiety that seems to have no rational basis.
Driving anxiety can become severe enough to prevent necessary transportation, as the person might experience panic attacks while driving, fear of losing control of the vehicle, or overwhelming anxiety about traffic situations. This can create practical problems with employment, healthcare access, or family responsibilities.
Financial decision-making often becomes impaired as anxiety interferes with the ability to think clearly about money management, bill paying, or financial planning. The person might avoid dealing with financial responsibilities due to anxiety, or make impulsive financial decisions to reduce immediate anxiety without considering long-term consequences.
Healthcare avoidance frequently occurs as medical appointments trigger intense anxiety about potential discovery of alcohol-related health problems or judgment from healthcare providers. This avoidance can prevent important medical care and allow alcohol-related health problems to progress without treatment.
The Social Isolation Consequence:
The combination of social anxiety, paranoid thinking, and overwhelming fear often leads to progressive social isolation that compounds other problems associated with alcoholism while eliminating potential sources of support and intervention.
Family relationship deterioration often occurs as anxiety makes normal family interactions feel overwhelming and threatening. The person might avoid family gatherings, become defensive during normal conversations, or withdraw from family activities due to anxiety that family members don't understand.
Friendship losses frequently result from the inability to maintain normal social interactions due to overwhelming anxiety. Friends might be avoided because social interaction feels too difficult, or relationships might be damaged by paranoid or defensive behavior during anxiety episodes.
Professional networking becomes impossible when work-related social interactions trigger intense anxiety, limiting career development opportunities and creating additional stress about job security and advancement.
Community involvement typically ends as anxiety makes participation in religious, civic, or recreational organizations feel overwhelming and threatening. This withdrawal eliminates important sources of meaning, purpose, and social support that could potentially assist with recovery.
Treatment Challenges and Considerations:
Addressing nameless fears and anxiety in alcoholism treatment requires specialized approaches that account for the neurochemical changes caused by chronic alcohol use and the complex relationship between anxiety symptoms and continued drinking.
Dual diagnosis treatment becomes essential when anxiety disorders co-occur with alcoholism, requiring simultaneous treatment of both conditions rather than addressing them separately. The anxiety symptoms may persist even after alcohol cessation and require ongoing psychiatric treatment and medication management.
Medication considerations become complex because many anxiety medications can be addictive and may not be appropriate for people with substance use disorders. However, some medications can be safely used to manage alcohol-related anxiety while supporting sobriety maintenance.
Cognitive-behavioral therapy specifically adapted for addiction-related anxiety can help people develop coping strategies for managing anxiety without alcohol while also addressing the distorted thinking patterns that contribute to paranoid and catastrophic thoughts.
Exposure therapy may be necessary to help people gradually re-engage with situations, places, and people that trigger anxiety, but this must be carefully coordinated with addiction treatment to prevent exposure to high-risk drinking situations.
The Recovery Process for Anxiety Symptoms:
Recovery from alcohol-related anxiety often requires patience and persistence, as neurochemical healing can take months or years and may require ongoing management even after sustained sobriety is achieved.
Neurochemical recovery involves gradual restoration of natural neurotransmitter functioning as the brain learns to produce adequate GABA, regulate glutamate activity, and restore normal stress response systems. This process can take 6-18 months or longer, requiring patience and often medication support during the healing period.
Confidence rebuilding becomes necessary as people learn to trust their ability to manage anxiety without alcohol while also rebuilding confidence in their ability to function in social and professional situations that previously triggered overwhelming fear.
Gradual exposure to previously avoided situations, places, and people often becomes necessary for full recovery, but this must be done carefully and with adequate support to prevent overwhelming anxiety that might trigger relapse.
Support group participation specifically focused on anxiety and addiction can provide peer support from others who understand the unique challenges of managing both conditions simultaneously.
The Family Perspective on Alcohol-Related Anxiety:
Family members often struggle to understand alcohol-related anxiety because the fears seem irrational and the anxiety seems to be "cured" by drinking, making it difficult to see anxiety as a legitimate medical condition rather than an excuse for continued alcohol use.
Education about anxiety disorders and their relationship to alcoholism becomes crucial for family members who need to understand that anxiety symptoms are real medical conditions requiring professional treatment rather than character weaknesses or manipulation tactics.
Accommodation vs. enabling becomes a delicate balance as family members try to support their loved one's anxiety management without inadvertently supporting continued alcohol use or preventing necessary treatment.
Family therapy often needs to address the confusion, frustration, and fear that family members experience when witnessing severe anxiety symptoms while also dealing with alcohol-related problems and their consequences.
Support for family members becomes important because living with someone experiencing severe anxiety and alcoholism creates significant stress that can affect the mental health and functioning of entire families.
Father Martin's identification of nameless fears and anxiety as a cardinal symptom of alcoholism was crucial because it helped people understand that their overwhelming anxiety and fears were not evidence of mental weakness or personal failure, but rather predictable consequences of how alcohol affects brain chemistry and psychological functioning. By recognizing anxiety as a medical symptom requiring professional treatment rather than a personal shortcoming requiring better self-control, individuals could seek appropriate dual diagnosis treatment that addressed both their addiction and their anxiety disorders simultaneously.
This understanding often provided enormous relief for people who had been struggling with overwhelming fear and anxiety that seemed to have no rational basis, helping them understand that their symptoms were real, treatable, and not evidence that they were "going crazy." The recognition that anxiety symptoms might persist even after alcohol cessation helped people prepare for the reality that recovery would require ongoing management of both conditions rather than the expectation that stopping drinking would automatically resolve all psychological distress.