Stages of Relapse
Breaking the Cycle: Understanding the Landscape of Relapse
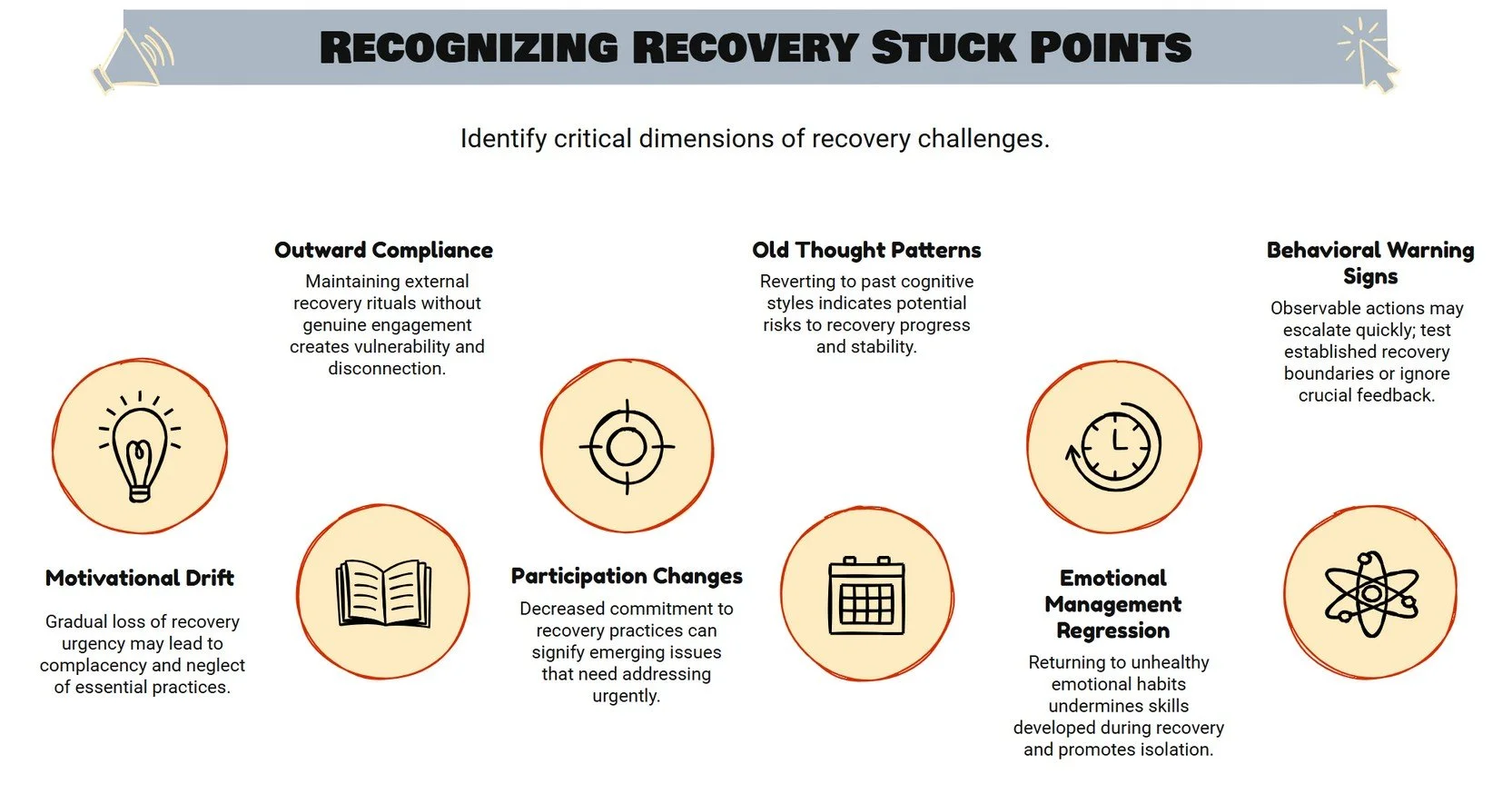
Hitting the Wall- Recovery Stuck Points
This self-assessment outlines seven critical dimensions of what appears to be recovery "stuck points" - warning signs that indicate someone's recovery process may be compromising before more obvious relapses occur. These dimensions represent subtle but significant shifts that can gradually undermine long-term recovery success.
Motivational Drift represents perhaps the most insidious challenge in sustained recovery. As time passes and the acute pain that initially drove someone to seek change fades from memory, the urgent necessity of recovery practices can begin to feel less compelling. This isn't a sudden shift but rather a gradual erosion where recovery moves from feeling essential to feeling optional. People may start questioning whether they really need to maintain certain practices, compare their progress to others in ways that minimize their own needs, or convince themselves they've somehow "outgrown" certain recovery requirements. This drift is particularly dangerous because it feels rational and graduated, making it difficult to recognize until significant ground has been lost.
Outward Compliance with Inner Disconnection creates a dangerous facade where someone maintains the external appearance of engaged recovery while internally disconnecting from its meaning and principles. This manifests as going through the motions without genuine engagement - attending meetings but not really participating, sharing what others want to hear rather than authentic experiences, or presenting a rosier picture of their recovery than they actually feel. The person may maintain recovery behaviors when others are watching but relax their standards when alone. This creates a split between their public recovery identity and their private experience, preventing authentic healing and creating significant vulnerability.
Program Participation Changes involve subtle shifts in how someone engages with their established recovery practices. What might start as occasional exceptions - skipping a meeting here, shortening a practice there - can gradually become a new, less committed pattern. The person may begin viewing recovery activities as less important, create increasingly elaborate justifications for reducing their commitments, or show up physically but disengage mentally. These changes often serve as early warning signs that precede more serious recovery compromises, making them crucial to recognize and address promptly.
Return to Old Thought Patterns represents a regression to pre-recovery thinking styles that initially contributed to addictive behaviors. This might include the resurgence of black-and-white thinking, believing they can now safely handle previously triggering situations, or developing increasingly self-centered perspectives. The person might start seeing themselves as a "special case" who doesn't need to follow the same recovery principles as others, or begin romanticizing past addictive behaviors while minimizing their consequences. These cognitive shifts are particularly concerning because they often precede behavioral changes and can be difficult to recognize without honest self-monitoring and sharing with others.
Emotional Management Regression occurs when someone returns to unhealthy patterns of dealing with emotions that were common before recovery. Instead of using the emotional processing skills developed in recovery, they might retreat to isolation during difficult times, suppress feelings rather than working through them appropriately, or use work, relationships, or other activities as emotional escape mechanisms. This regression might also manifest as increasing emotional volatility or numbness, along with decreased willingness to be vulnerable about struggles with trusted supports.
Behavioral Warning Signs represent the observable actions that often follow changes in thinking and emotional management. These might start small but can escalate quickly if not addressed. Common signs include testing previously established recovery boundaries, seeking out relationships or situations that undermine rather than support recovery, or engaging in substitute compulsive behaviors. The person might become defensive when others express concern about these changes, or start making impulsive decisions without considering their impact on recovery stability.
Secret Life Development represents perhaps the most serious dimension, involving the creation of compartmentalized life areas that remain hidden from recovery supports and community. This secretive behavior prevents the transparency and accountability that are essential for sustained recovery. Warning signs include keeping important life areas separate from recovery community involvement, lying or omitting important truths about behaviors and choices, or maintaining a facade of wellness while privately struggling with significant challenges. The development of secrets creates internal division and prevents the integration necessary for authentic healing.
Understanding these dimensions is crucial because they often develop gradually and can seem reasonable or justified in the moment. By recognizing these patterns early, individuals in recovery and their support systems can intervene before more serious consequences develop, recommitting to the practices and principles that support long-term recovery success.
Stress Reactions vs Stress Response
This self-assessment outlines seven critical dimensions of stress reactions that are particularly relevant for individuals in recovery, highlighting how stress can create vulnerabilities that threaten recovery stability. These dimensions help identify specific patterns that require attention and intervention to maintain recovery success during challenging periods.
Stress Perception and Awareness represents a fundamental challenge in recovery, as many individuals have compromised abilities to accurately recognize and assess their stress levels. Years of substance use or addictive behaviors often numb natural stress detection systems, making it difficult to gauge when stress has reached concerning levels. Some people may only recognize stress through physical manifestations like headaches or muscle tension, while others might minimize dangerous stress levels or be genuinely surprised when others point out their obvious stress signals. There's often a pattern of pushing through warning signs rather than responding appropriately, along with difficulty distinguishing between normal, manageable stress and stress levels that require intervention. Developing accurate stress perception becomes foundational to recovery because without it, people cannot take appropriate protective action when stress threatens their stability.
Concealment Behaviors involve the deliberate hiding of stress levels and struggles from others, often stemming from shame about not handling stress "better" or fear of being judged as failing in recovery. This pattern typically includes presenting a calm exterior while experiencing significant internal turmoil, withdrawing from connections precisely when support is most needed, or responding defensively when others express legitimate concern about visible stress signs. People may create elaborate excuses to avoid recovery activities during high stress periods or compartmentalize their "recovery life" from their "stress life" as if they were separate entities. While these concealment behaviors often feel protective and are usually well-intentioned, they create dangerous isolation and prevent access to crucial support systems exactly when they're most needed for maintaining recovery stability.
Functional Impairment provides concrete, observable indicators that stress has exceeded healthy limits and is beginning to compromise daily functioning. This dimension is particularly valuable because it offers objective measures that are harder to minimize or deny. Sleep disruption often appears early, including difficulty falling asleep, staying asleep, or waking much earlier than usual. Concentration and decision-making abilities deteriorate, making work or daily responsibilities more challenging. Self-care routines that normally anchor recovery stability may begin to slip, productivity decreases, and people may start missing obligations or appointments. Memory problems and general disorganization also signal that stress has reached levels requiring intervention. Monitoring these functional impacts provides concrete evidence of when stress management strategies need to be intensified or additional support sought.
Emotional Dysregulation involves the loss of emotional balance during stress, which can manifest in various ways that compromise recovery stability. Some people experience rapid mood shifts, moving from calm to agitated to despairing within short periods. Emotional intensity and reactivity often increase, with responses becoming disproportionate to triggering events. Others may alternate between emotional numbing and overwhelming feelings, or cycle between feeling invincible and completely hopeless. This dysregulation is particularly concerning in recovery because emotional balance is crucial for making sound decisions and maintaining healthy coping strategies. The unpredictability of these emotional states can also strain relationships and recovery supports, creating additional stress that compounds the original problem.
Physical Manifestations represent the body's expression of stress states and often provide the earliest warning signals before conscious awareness of stress emerges. These somatic responses are particularly important to recognize because they offer opportunities for early intervention. Common manifestations include tension-related symptoms like headaches, jaw clenching, or muscle pain, especially in the neck and shoulders. Digestive disturbances may appear as appetite changes, stomach pain, or nausea. Energy patterns often shift, with people experiencing fatigue despite adequate rest, or conversely, feeling wired and unable to relax. Breathing patterns may become shallow, rapid, or irregular, and immune system functioning can be compromised, leading to increased susceptibility to illness. Learning to recognize these physical signals allows for proactive stress management before emotional or behavioral complications develop.
Internal Recognition with External Denial creates a particularly dangerous gap between inner knowing and outer expression. In this pattern, people internally recognize that their stress levels are problematic and potentially threatening to their recovery, but simultaneously deny or minimize this reality to others and sometimes even to themselves. They may hear an inner warning voice telling them they need help but convince themselves to handle everything alone. This often stems from worry about judgment if stress struggles are acknowledged, unfavorable comparisons to others who appear to manage stress better, or fear that admitting stress signals failure in recovery. This internal-external split prevents appropriate response to accurate internal signals and creates significant vulnerability by blocking access to support and intervention when they're most needed.
Recovery Program Impact addresses how stress specifically affects engagement with recovery practices and communities, often leading to disengagement precisely when these supports are most crucial. During high stress periods, commitment to recovery practices frequently weakens, with people questioning whether recovery tools actually apply to their current situation or are effective for managing the specific stressors they're facing. Thoughts about substances or addictive behaviors may increase as old coping mechanisms seem more appealing during difficult times. There's often distancing from recovery community and supports, along with elaborate justifications for skipping meetings, therapy sessions, or other recovery activities. This pattern is particularly dangerous because it removes protective factors exactly when they're most needed, creating a cycle where reduced recovery engagement leads to increased vulnerability, which then leads to even greater stress and further disengagement.
Understanding these stress reaction dimensions allows individuals in recovery and their support systems to develop targeted strategies for recognizing and addressing stress before it compromises recovery stability. Each dimension offers specific intervention points and helps identify when professional help or intensified support may be necessary to maintain recovery progress.
Denial Regression
This self-assessment explores seven critical dimensions of denial that can emerge during the recovery process, representing sophisticated psychological mechanisms that can undermine recovery stability often before the individual or their supports fully recognize the danger. These denial patterns are particularly insidious because they can develop gradually and often feel rational or justified, making them difficult to identify and address.
Recovery Practice Abandonment serves as the behavioral foundation upon which other denial patterns often build. This dimension involves the gradual reduction or complete elimination of activities and connections that previously supported sobriety and recovery stability. The process typically begins innocuously finding reasonable excuses to skip a recovery meeting here or there, gradually reducing time spent on daily recovery practices like meditation or journaling, or postponing regular check-ins with sponsors or recovery supports. Over time, recovery activities begin to feel less necessary than they once did, and other life activities start taking priority over recovery commitments. The dangerous aspect of this pattern is how each individual change seems minor and justifiable, while the cumulative effect significantly undermines the foundation of recovery stability. As distance from recovery practices increases, it creates psychological space for other denial patterns to emerge and flourish.
"Cured" Thinking Patterns represent perhaps the most dangerous cognitive shift in recovery, involving the belief that addiction was a temporary condition that can be fully resolved, thereby eliminating the need for ongoing recovery maintenance. This perspective directly contradicts the well-established understanding of addiction as a chronic condition requiring continuous management. These thought patterns often emerge after periods of stable recovery when the acute memory of addiction consequences has faded and recovery benefits have become so normalized that they're taken for granted. The individual may begin entertaining ideas that their addiction was merely a temporary problem they've overcome, question whether long-term recovery practices are really necessary, or start comparing themselves favorably to "real" addicts who they perceive as more severely affected. This thinking often progresses to minimizing the severity of past addiction experiences and may even lead to considering experiments with controlled substance use or engaging in previously addictive behaviors "just to prove" they're cured.
Communication Breakdown involves the deterioration of honest disclosure to recovery supports, interrupting the essential recovery practice of transparency that maintains connection and accountability. This pattern creates dangerous isolation even while maintaining the superficial appearance of ongoing connection with recovery community and supports. The breakdown typically manifests as withholding important information about concerning thoughts, feelings, or experiences, presenting a more positive picture of recovery than is honestly felt, or saying what others want to hear rather than sharing authentic experiences. Communication becomes increasingly selective, with individuals omitting details that might concern others or using deliberately vague language to avoid direct honesty about their internal experience. This dimension demonstrates how denial operates interpersonally, creating barriers to the authentic connection that supports recovery while maintaining a facade of continued engagement.
Internal Warning System represents a crucial dimension that actually works in favor of recovery—the moments of clarity when individuals recognize concerning changes in their own recovery process. These warning signals represent the part of the person that remains committed to recovery and notices when denial patterns are beginning to emerge. This system often manifests as recognition of worrisome changes in thinking patterns, concern about shifts in emotional responses to recovery-related situations, or awareness that problematic behavior patterns from before recovery are beginning to reemerge. There may be moments of clarity about drift from recovery principles or feelings of internal conflict about the overall direction of their recovery. This dimension represents an important psychological resource—the capacity to recognize denial even as it begins to operate—that can be leveraged to intervene before significant relapse progression occurs. However, this warning system is often overridden by other denial dimensions.
Fear of Judgment creates powerful motivation to conceal concerning patterns rather than seeking help with them, as individuals anticipate negative responses from others if recovery struggles were honestly disclosed. This fear typically appears as worry about how others might react to current thoughts or struggles, anticipation of criticism if questions about recovery are shared with supports, or expectation of rejection if struggles are revealed honestly. There's often fear of disappointing those who view the person's recovery positively or have invested emotionally in their success. This leads to avoiding vulnerable sharing due to expected negative responses, creating a self-fulfilling prophecy where isolation increases actual vulnerability. This dimension reflects how social concerns can powerfully reinforce denial patterns by discouraging the honest disclosure that might interrupt them, even when the feared judgments may be largely imagined or exaggerated.
Rationalization Processes involve the creation of elaborate explanations that justify concerning recovery choices while maintaining a positive self-image. These sophisticated cognitive distortions allow problematic patterns to continue by reframing them as reasonable, necessary, or even beneficial developments. Common patterns include creating complex explanations for choices that would have been clearly problematic earlier in recovery, reframing obvious warning signs as positive developments or signs of growth, or engaging in self-convincing internal dialogue that everything is fine despite mounting contrary evidence. When others express concern, these concerns are dismissed as overreactions or misunderstandings. Perhaps most dangerously, individuals begin developing reasons why general recovery principles don't apply to their specific situation, creating a sense of being exceptional or beyond the need for standard recovery practices. This dimension reflects how the thinking process itself becomes compromised in service of maintaining the possibility of returning to addictive behaviors.
Internal Recovery Debate represents perhaps the most psychologically complex dimension, involving the experience of competing internal voices or perspectives—one aligned with recovery values and commitments, and another representing addiction thinking and desires. This internal conflict often represents a late stage in denial progression, where the fundamental commitment to recovery itself is being actively questioned and debated internally. Signs include experiencing distinctly competing internal voices about recovery needs, finding oneself arguing against previously held recovery wisdom, or oscillating between recovery-oriented and addiction-oriented perspectives sometimes within the same day or even the same conversation. Increasing mental energy becomes devoted to questioning recovery principles that were once accepted without debate, and internal negotiations begin about previously firm recovery boundaries. This dimension reflects the profound psychological conflict that emerges as denial progresses toward its most dangerous stages, often preceding conscious consideration of relapse and representing a critical intervention point where intensive support and professional help are typically necessary to prevent progression to actual substance use or addictive behaviors.
Understanding these denial dimensions is crucial because they represent sophisticated psychological processes that can feel entirely rational and justified to the person experiencing them, while simultaneously creating significant risk for recovery failure. Early recognition of these patterns by individuals, their families, and recovery supports can enable intervention before more serious consequences develop.
Addiction Protection Perception
This self-assessment explores seven critical dimensions of addicted belief systems that can reemerge during recovery, representing sophisticated cognitive shifts that can gradually undermine recovery stability by reactivating thought patterns that originally supported addictive behaviors. These belief dimensions are particularly dangerous because they often feel logical and reasonable to the person experiencing them, while simultaneously creating psychological pathways back toward substance use or addictive behaviors.
Stress-Activated Belief Shifts highlight the vulnerable relationship between stress and cognitive stability in recovery. During periods of elevated stress or significant life challenges, the recovery-oriented cognitive frameworks that normally guide thinking and decision-making can become weakened, allowing dormant addiction-supportive belief systems to reactivate. This manifests as noticeable changes in thinking about recovery during stressful periods, with individuals beginning to question previously accepted recovery principles when facing difficulties. They may start doubting the value of recovery practices during challenging circumstances, find their thinking patterns reverting to perspectives they held during active addiction, or experience weakening commitment to recovery beliefs as stress levels increase. This dimension is particularly concerning because stress is an inevitable part of life, and if belief systems become unstable under pressure, it creates recurring vulnerability throughout the recovery process. Understanding this relationship between stress and belief system activation becomes crucial for developing protective measures and intensified support during vulnerable periods.
Powerlessness Questioning involves a fundamental challenge to one of recovery's core concepts—the acknowledgment of powerlessness over addiction. This shift represents a return to pre-recovery thinking that minimizes the severity of addiction while maximizing beliefs about personal control and capability. Common manifestations include reconsidering whether true addiction was actually present or whether past difficulties were just a challenging phase that's now resolved. Individuals may begin thinking that their past problems with substances were exaggerated by themselves or others, or start believing that addiction was primarily circumstantial rather than representing a fundamental condition requiring ongoing management. They might find themselves thinking that their personal control over substance use was greater than they previously admitted, leading to questioning whether complete abstinence is truly necessary for their situation. This dimension is particularly dangerous because it directly undermines the foundational recognition that led to recovery in the first place, creating significant vulnerability to resumed use by convincing the person that they never really lost control or that they've now regained sufficient control to manage their relationship with substances.
Moderation Fantasies represent some of the most seductive and dangerous cognitive shifts in recovery, involving elaborate beliefs that controlled, occasional, or limited substance use might now be possible despite extensive previous evidence to the contrary. These fantasies often emerge after periods of stable recovery when the acute memory of addiction consequences has faded and confidence has grown. They typically involve entertaining detailed thoughts about how controlled or occasional substance use could work, believing that sufficient learning and growth have occurred to enable moderate use that was previously impossible. The person may focus selectively on alleged examples of others who successfully returned to controlled use while ignoring the much more common stories of failed moderation attempts. They create mental scenarios about how personal limits could be set and maintained with substances, often involving elaborate rules and safeguards that feel convincing internally. This dimension reflects the addicted mind's remarkable capacity to create seemingly logical justifications for returning to use while engaging in selective memory that minimizes or forgets past evidence against such possibilities.
Program Necessity Doubts involve questioning whether ongoing recovery practices and program involvement remain essential after achieving initial stability, reflecting a dangerous tendency to view recovery as a time-limited intervention rather than an ongoing way of life. This dimension often emerges after individuals have experienced significant recovery benefits and begin to take their stability for granted. Common patterns include questioning whether ongoing recovery practices truly remain essential, believing they've somehow "graduated" from needing certain recovery components, or thinking that sufficient time in recovery justifies reduced program involvement. Individuals may consider whether their personal recovery needs differ from general program recommendations, or find themselves believing that recovery can be maintained with minimal ongoing program participation. This dimension undermines the recovery foundation by challenging the ongoing nature of the healing process and the continuing need for structured support, often leading to gradual disengagement from the very practices and connections that created and maintain recovery stability.
Self-Perception Distortions involve the development of increasingly inaccurate views of oneself, particularly regarding capabilities, vulnerabilities, and ongoing recovery needs. These distortions can manifest as either unrealistic grandiosity or excessive self-criticism, both of which undermine recovery-supportive perspectives in different ways. Typical distortions include views of personal capabilities becoming either unrealistically positive or negative, losing accurate perspective on continuing vulnerability to addiction, or developing inflated confidence in the ability to resist triggers and handle challenging situations. Individuals may begin perceiving themselves as fundamentally different from others in recovery—either as more capable of managing addiction independently or as so different that standard recovery approaches don't apply. Their understanding of their own motives and behaviors may become less accurate over time as self-serving interpretations replace honest self-assessment. These self-perception distortions create vulnerability through either overconfidence that leads to risky situations or despair that undermines motivation to maintain recovery practices.
Recovery Distortion involves developing increasingly inaccurate perceptions of the recovery process itself, its requirements, and what constitutes genuine recovery health. These perceptions typically shift in self-serving directions that gradually accommodate the possibility of future substance use. Common distortions include beginning to view standard recovery requirements as excessive, unnecessary, or overly cautious for someone with their level of stability. Perceptions of what constitutes recovery health may become unrealistic, with individuals redefining recovery success in ways that might eventually accommodate controlled use or reduced vigilance. Recovery practices that were once viewed as essential supports may be reframed as obstacles to "normal living" or as signs that true recovery hasn't been achieved. The understanding of the recovery process itself becomes increasingly self-serving, often involving the belief that real recovery should eventually allow for a "normal" relationship with substances or that continuing recovery practices indicates incomplete healing rather than ongoing maintenance of health.
Belief System Rigidity represents the protective mechanism by which addicted thinking shields itself from examination and correction. This dimension involves decreasing flexibility and openness regarding personal thinking patterns, particularly strong resistance to examining emerging beliefs that contradict established recovery principles. This rigidity often manifests as increasing defensiveness when questionable thinking is identified by others, whether family members, sponsors, therapists, or recovery community members. Signs include becoming less willing to question one's own thinking even when it clearly contradicts previously held recovery beliefs, defending new perspectives even when they undermine recovery principles, or dismissing feedback that challenges emerging belief shifts. Thinking may become increasingly absolutist or black-and-white, losing the nuanced perspective that healthy recovery typically develops. There's often strong resistance to examination of belief system changes even when trusted others express legitimate concern. This dimension is particularly dangerous because it isolates the person from recovery-supportive perspective and feedback, creating a closed system where addicted thinking can develop without challenge or correction, ultimately leading to beliefs and decisions that support eventual return to addictive behaviors.
Understanding these addicted belief dimensions is crucial because they represent the cognitive foundation that typically precedes behavioral relapse, often developing gradually over time in ways that feel entirely reasonable and justified to the person experiencing them. Recognition of these patterns by individuals in recovery, their support systems, and treatment professionals can enable early intervention before these belief shifts translate into actual substance use or other addictive behaviors.
Internal Conflict & Relapse Justification
This self-assessment outlines twelve critical dimensions of self-defeating thinking patterns that can significantly undermine recovery efforts, representing sophisticated cognitive distortions that gradually erode the mental foundation necessary for sustained sobriety. These thinking patterns are particularly dangerous because they often feel rational and justified to the person experiencing them, while systematically creating psychological vulnerabilities that can lead to relapse.
Negative Recovery Evaluation involves a fundamental shift in how individuals assess their recovery experience, moving from viewing recovery as beneficial to seeing it as burdensome or questionably worthwhile. This pattern manifests as questioning whether recovery is "worth it" compared to the ongoing effort required, focusing disproportionately on recovery challenges while minimizing or forgetting the benefits and improvements that have occurred. Individuals may compare their recovery experience unfavorably to others who seem to have easier or more successful journeys, or begin thinking primarily about how recovery restricts their choices rather than how it has freed them from the consequences of addiction. They often evaluate their recovery progress against unrealistic expectations, setting standards that guarantee disappointment and frustration. This evaluation process creates significant vulnerability by gradually eroding the motivation and commitment necessary for sustained recovery efforts, making it increasingly difficult to justify or maintain the ongoing work that recovery requires.
Relapse Justification represents the cognitive preparation for potential return to substance use by creating elaborate scenarios and exceptions that would make substance use appear acceptable or reasonable. This dangerous pattern involves developing specific circumstances where substance use would be justified—perhaps during celebrations, crises, or after achieving certain milestones. Individuals may create "exceptions" to their recovery commitment for particular situations, or develop beliefs that they've somehow "earned" the right to use substances after periods of sustained sobriety. They begin emphasizing personal choice and autonomy while systematically minimizing the potential consequences of what they frame as "controlled" or "occasional" use. This justification process creates profound vulnerability by weakening the cognitive barriers against relapse and developing permission-giving beliefs that make substance use appear not only acceptable but reasonable under certain conditions, essentially creating a mental pathway back to active addiction.
Distorted Self-Perception involves developing a fundamentally negative and inaccurate view of oneself that becomes incompatible with sustained recovery success. Common distortions include seeing oneself as fundamentally flawed, broken beyond repair, or inherently different from others who successfully maintain recovery. Individuals may believe they don't deserve happiness, success, or the benefits that recovery can provide, often comparing themselves unfavorably to others in recovery while defining themselves primarily by past mistakes and failures rather than current efforts and growth. They struggle to recognize their own strengths, accomplishments, and progress in recovery, instead maintaining a persistently negative self-image. This distortion creates vulnerability by generating shame, hopelessness, and a deep sense of unworthiness that undermines belief in the possibility of sustained recovery success, often becoming a self-fulfilling prophecy where negative self-perception leads to behaviors that confirm the distorted beliefs.
Catastrophic Thinking involves systematically magnifying difficulties beyond their actual proportions and interpreting manageable situations as overwhelming crises. This pattern manifests as interpreting minor setbacks—such as having a difficult day or making a small mistake—as major recovery failures that indicate fundamental problems. Temporary challenges are viewed as permanent conditions, and individuals believe that if recovery isn't proceeding perfectly, it must be failing entirely. They frequently imagine worst-case scenarios about their recovery future, seeing temporary emotional discomfort or challenges as permanent states of being rather than normal fluctuations in the recovery process. This thinking creates profound vulnerability by generating overwhelming distress about situations that are actually manageable and creating a sense that recovery challenges are insurmountable, often leading to abandonment of recovery efforts in the face of normal difficulties.
All-or-Nothing Thinking eliminates the nuanced middle ground where sustainable recovery actually exists, instead viewing recovery situations in extreme, black-and-white terms. Individuals see themselves as either totally successful or completely failing in recovery, with no recognition of partial successes, gradual progress, or the normal ups and downs of the recovery process. They believe that if recovery can't be done perfectly, it shouldn't be attempted at all, setting impossible standards that guarantee perceived failure. This extends to viewing other people and situations in extreme terms as well—believing that people either completely support or totally oppose their recovery, or perceiving challenges as either completely manageable or utterly overwhelming. This thinking pattern creates vulnerability by establishing unrealistic standards that ensure disappointment and eliminate recognition of the incremental progress that characterizes healthy recovery.
Impulsive Thought Patterns undermine the deliberate, reflective decision-making that sustainable recovery requires by prioritizing immediate responses over thoughtful consideration. These patterns involve making significant recovery-related decisions without adequate consideration of consequences, reacting to challenges with immediate, unplanned responses rather than taking time to develop appropriate strategies. Individuals struggle with delaying gratification for long-term benefits, often abandoning recovery plans when they don't yield immediate results, and have difficulty following through with commitments that require sustained effort over time. This impulsivity creates vulnerability by bypassing the reflective thinking necessary for wise recovery choices and consistently prioritizing immediate relief or gratification over the long-term stability that recovery provides.
Compulsive Thought Patterns create persistent cognitive pressure toward substance-related thinking and behaviors that can eventually overwhelm psychological resistance to relapse. These patterns involve experiencing intrusive thoughts about substance use that can't easily be dismissed or controlled, feeling drawn to repetitive behaviors despite knowing they have negative consequences, and engaging in mental rituals or obsessive thinking patterns to manage recovery-related anxiety. Individuals may feel driven by thoughts that create unnecessary distress and experience thinking patterns that feel beyond their control, creating a sense of being at the mercy of their own cognitive processes. This creates vulnerability by generating persistent preoccupation with substances and related behaviors that gradually wears down resistance and commitment to recovery.
Self-Sabotage Beliefs involve unconsciously creating conditions that undermine recovery success, often generating preventable problems that then justify abandoning recovery efforts. This pattern manifests as engaging in behaviors known to create future difficulties, setting up situations where failure becomes more likely than success, or making recovery unnecessarily complicated or difficult. Individuals may invite chaos or crisis into otherwise stable recovery periods, creating drama or problems that drain recovery resources and energy. These beliefs create vulnerability by systematically generating situations that make recovery more challenging than necessary and creating conditions where relapse begins to appear reasonable or even inevitable as a response to self-created difficulties.
Emotional Reasoning allows temporary and fluctuating emotional states to override stable recovery commitments and rational decision-making. This pattern involves making important recovery decisions based primarily on feelings rather than rational consideration of consequences, trusting negative emotions more than positive ones when making choices, and interpreting emotional discomfort as evidence that recovery isn't working properly. Individuals may believe that feeling like using substances predicts that they will eventually use, or make their recovery commitments contingent on their current emotional state rather than on stable values and long-term goals. This reasoning creates vulnerability by allowing unpredictable emotional fluctuations to determine crucial recovery decisions rather than the consistent commitment and rational planning that sustainable recovery requires.
Future Discounting systematically minimizes the long-term benefits of recovery while overvaluing immediate but temporary relief, creating a distorted cost-benefit analysis that favors short-term gratification over long-term stability. This pattern involves valuing immediate relief more highly than substantial long-term benefits, having difficulty connecting current recovery actions to future positive outcomes, and making choices that prioritize short-term comfort over long-term well-being. Individuals minimize the future consequences of recovery-compromising decisions while struggling to maintain motivation for delayed rewards, essentially becoming unable to accurately weigh the true costs and benefits of recovery versus relapse. This creates vulnerability by systematically undervaluing everything that makes recovery worthwhile while overvaluing the temporary relief that substances might provide.
Responsibility Distortion shifts accountability away from oneself, undermining the sense of personal agency essential for sustained recovery action. This pattern involves blaming others for recovery challenges rather than examining one's own role, attributing recovery successes to luck, circumstances, or other people's efforts rather than recognizing personal effort and growth. Individuals see themselves primarily as victims of circumstances rather than agents of change, expect others to manage recovery challenges they could address personally, and fail to recognize their own role in creating recovery-related problems. This distortion creates vulnerability by undermining the personal responsibility and self-efficacy that are fundamental to maintaining recovery over time.
Recovery Resistance generates automatic opposition to recovery-supporting ideas and guidance, creating unnecessary isolation from helpful resources and approaches. This pattern involves finding oneself arguing against recovery suggestions or guidance even when they might be beneficial, focusing on reasons why recovery approaches won't work rather than how they might be helpful, and maintaining a stance of knowing better than those with successful long-term recovery. Individuals may reject potentially valuable recovery support based on minor disagreements or differences, and mentally rehearse arguments against established recovery principles or practices. This resistance creates vulnerability by preventing the integration of potentially helpful recovery approaches and creating unnecessary isolation from the supportive guidance that could strengthen recovery efforts.
Understanding these self-defeating thinking dimensions is crucial because they represent the cognitive foundation that typically undermines recovery from within, often developing gradually and feeling entirely justified to the person experiencing them. Recognition of these patterns enables early intervention before they translate into behaviors that compromise recovery stability.
Shift to Use Urges
This self-assessment explores seven critical dimensions of urges that individuals face during recovery, representing complex psychological and physiological responses that can threaten recovery stability if not properly understood and managed. These urge dimensions reflect the profound ways that addiction rewires both brain chemistry and psychological associations, creating persistent challenges that require ongoing attention and specific management strategies.
Deprivation Anxiety represents one of the most fundamental and persistent challenges in recovery, involving the deeply distressing belief that sobriety means permanent loss of pleasure, connection, or effective coping ability. This dimension reflects how addiction creates a profound distortion in perception where substances are viewed as essential sources of fulfillment rather than recognized as agents of destruction. Common manifestations include a persistent feeling of missing out on enjoyment or pleasure due to sobriety, with individuals believing that substances are necessary components of a full or satisfying life. They may experience significant anxiety when contemplating permanent abstinence, feel a sense of loss when observing others using substances socially, and perceive sobriety as punishment rather than the liberation it actually represents. This anxiety often persists well into recovery because it reflects fundamental beliefs about what makes life worthwhile and manageable. Addressing this dimension requires active challenge to the underlying distorted belief system that substances provide genuine benefits worth the devastating cost of addiction, along with patient development of authentic sources of pleasure, connection, and coping that don't require chemical alteration.
Boredom with Sobriety involves experiencing recovery as mundane, lacking excitement, or devoid of meaningful engagement, reflecting how addiction fundamentally rewires reward systems to respond intensely to substances while simultaneously diminishing capacity to appreciate natural rewards and experiences. This experience typically manifests as finding recovery routine or lacking the excitement that characterized periods of active substance use, with individuals comparing the perceived intensity and stimulation of using days to the apparent flatness of recovery. They may think that nothing genuinely interesting happens in sobriety, believe that substances are necessary for true enjoyment, creativity, or fun, and struggle to find meaningful engagement in activities that don't provide artificial stimulation. This dimension is particularly challenging because it reflects genuine neurological changes where the brain's reward system has been hijacked by substances, requiring both time for neurological healing and active cultivation of authentic engagement with life on its own terms. Recovery from this boredom requires patience with the healing process while actively developing new sources of genuine interest and engagement that can eventually provide satisfaction comparable to or exceeding what substances appeared to offer.
Pleasure Memories and Associations involve experiencing intrusive, selective recollections of past substance use that emphasize pleasurable aspects while systematically minimizing or completely omitting negative consequences and devastating outcomes. These distorted memories can trigger powerful urges through their associated emotional and physical responses, creating a romanticized version of addiction that bears little resemblance to actual lived experience. This pattern typically includes intrusive positive memories of substance use that seem to arrive unbidden, selective remembering of pleasurable aspects while the mind conveniently forgets consequences, and active romanticizing of using experiences in current thoughts and fantasies. Individuals may experience strong physical responses when recalling past use—including excitement, anticipation, or even physical sensations—and find themselves mentally rehearsing scenarios of using again "successfully" this time. Managing this dimension requires developing reality-based memory correction practices that incorporate complete rather than selective recall of addiction experiences, including systematic remembrance of consequences, losses, and pain that addiction caused. This often involves writing exercises, discussion with others who witnessed the full reality of one's addiction, and deliberate practices that counter the brain's tendency to remember only positive aspects while forgetting negative ones.
Emotional Triggers involve the powerful connection between specific emotional states and urges to use substances, reflecting how substances often became the primary or exclusive method for managing emotions during active addiction. This creates profound associations between particular feeling states and substance-seeking behavior that can persist long into recovery. Common emotional triggers include anxiety or stress that automatically trigger thoughts of using substances for relief, sadness or depression that leads to cravings for mood alteration, and anger or frustration that creates urges to escape uncomfortable feelings through chemical means. Perhaps surprisingly, positive emotional states like joy or excitement can also trigger desires to "enhance" or celebrate experiences with substances. Individuals often struggle with managing any form of emotional discomfort without immediately considering substances as a solution. Addressing this dimension requires developing comprehensive alternative emotional management strategies for each challenging emotion that commonly triggers urges, practicing these strategies consistently until they become more automatic than substance-seeking responses, and building tolerance for emotional discomfort without immediate chemical relief.
Environmental and Social Triggers involve external situations, settings, people, or cues that activate urges to use through powerful conditioning and association processes that create lasting neural pathways established during active addiction. These triggers can create surprisingly powerful responses even after extended periods of recovery because they connect directly to deeply ingrained neural patterns. Typical triggers include specific locations or settings where substance use occurred that can immediately activate cravings, presence of others who are actively using substances that creates strong urges through social modeling and availability, sight of substances or related paraphernalia that triggers immediate craving responses, and certain times, days, or occasions that became associated with substance use patterns. Even media depictions of substance use can activate wanting and craving responses in vulnerable individuals. Managing this dimension requires a thoughtful combination of strategic avoidance where appropriate and realistic, preparation for unavoidable exposure through specific coping strategies, and gradual desensitization through repeated exposure without use that can eventually weaken these conditioned responses over time.
Physical and Sensory Triggers operate through both psychological association and physiological memory, involving bodily sensations or sensory experiences that activate urges through their connection to substance effects or use rituals. These triggers can be particularly challenging because they often occur without warning and connect to deep physical memories of substance experiences. Common physical and sensory triggers include specific physical sensations that are reminiscent of substance effects and immediately trigger desire to recreate those feelings, particular tastes, smells, or sounds that were associated with substance use and now activate craving responses, and physical discomfort or pain that creates automatic desires to self-medicate with substances. Fatigue or exhaustion can significantly increase vulnerability to all types of urges, while hunger or other unaddressed physical needs can intensify urge experiences when basic self-care is neglected. Addressing this dimension requires both consistent proper physical self-care to reduce overall vulnerability and development of specific strategies for managing unavoidable physical and sensory triggers when they occur, often including mindfulness practices that allow individuals to observe and tolerate physical sensations without immediately seeking chemical alteration.
Urge Progression involves the critical understanding that untreated urges tend to intensify and expand over time rather than naturally diminishing, potentially leading to relapse if not effectively addressed through appropriate intervention. This progression often follows predictable patterns that can be identified and interrupted at early stages when management is significantly easier. Signs of urge progression include urges that begin subtly but systematically intensify if not directly addressed, patterns where occasional urges become increasingly frequent over time, and unaddressed urges that lead to more elaborate and detailed fantasies about using substances. The intensity of urges often correlates directly with decreasing participation in recovery activities, and there's typically a strong connection between isolation from recovery supports and increasing urge strength. Understanding this progression is crucial because it allows for early intervention at stages where urges are much more manageable, preventing escalation to points where resistance becomes significantly more difficult and relapse risk increases dramatically. This knowledge empowers individuals to take urges seriously from their earliest emergence rather than hoping they will simply disappear on their own, and to implement appropriate coping strategies before urge intensity reaches overwhelming levels.
Understanding these urge dimensions is essential for developing comprehensive relapse prevention strategies because each dimension requires specific approaches and interventions. Recognition of these patterns allows individuals in recovery and their support systems to develop targeted responses that address the particular challenges each type of urge presents, ultimately building resilience against the complex psychological and physiological pull toward substance use that characterizes the recovery process.
Disconnection, Avoidance & Social Isolation
This self-assessment explores seven critical dimensions of social isolation that can emerge during recovery, representing subtle but dangerous patterns that gradually remove the interpersonal supports essential for maintaining sobriety. These isolation dimensions are particularly insidious because they often develop gradually and can feel natural or justified, while systematically dismantling the social foundation that recovery requires to remain stable over time.
Recovery Support Avoidance involves the gradual but deliberate disconnection from individuals who actively support recovery goals and values, often beginning with seemingly minor changes that escalate into persistent avoidance patterns. This dimension typically starts subtly with occasional declined invitations to recovery-related social activities, delayed responses to calls or messages from recovery supports, or finding small excuses to avoid spending time with people who are committed to sobriety. Over time, individuals may begin feeling genuinely uncomfortable or irritated when around people who are actively engaged in recovery, leading to more deliberate screening of calls or avoidance of contact with recovery mentors, sponsors, or other supportive figures. They may consistently find reasons to leave recovery gatherings early, arrive late, or avoid them altogether. This avoidance creates profound vulnerability by systematically removing essential accountability, perspective, and encouragement precisely when these supports are most needed for maintaining recovery stability. The isolation from recovery-supportive relationships often occurs at the exact moment when connection with these individuals could provide crucial intervention and support to prevent further deterioration.
Recovery Activity Disengagement represents the behavioral component of isolation, involving systematic withdrawal from both structured and unstructured activities that previously supported recovery stability and provided meaningful engagement with sober living. This pattern typically includes participating less frequently in activities that were central to early recovery success, gradually reducing involvement in recovery-oriented social events that once provided connection and reinforcement, and stopping engagement in healthy recreational activities that were discovered and enjoyed during recovery. Recovery activities begin to feel like burdensome obligations rather than supportive resources, and individuals find increasingly elaborate reasons why recovery-supportive activities are no longer necessary for their particular situation. This disengagement systematically removes important protective factors from daily life, creating increasing vulnerability as the recovery-reinforcing experiences that once anchored stability become less frequent or disappear entirely. The loss of these activities also removes structure, meaning, and positive social connection that recovery requires for long-term sustainability.
Professional Support Disconnection involves withdrawing from structured therapeutic relationships with counselors, therapists, psychiatrists, or other treatment professionals, often reflecting underlying resistance to accountability and external perspective from trained observers who might identify concerning patterns. This dimension commonly manifests as frequently canceling or rescheduling therapy or counseling appointments, attending professional support sessions but participating only minimally when present, or systematically withholding important information from treatment professionals about thoughts, feelings, or behaviors that might be concerning. Individuals often convince themselves that they have progressed beyond needing professional support or begin questioning the value or effectiveness of professional treatment altogether. This disconnection represents the loss of objective professional guidance that is specifically trained to identify and address emerging concerns before they develop into full crises. Professional supports often provide the external perspective and specialized knowledge that individuals cannot provide for themselves, making their loss particularly dangerous during vulnerable recovery periods.
Recovery Meeting Withdrawal involves decreasing engagement with recovery mutual aid groups such as AA, NA, or other recovery communities, either through significantly reduced attendance or notably diminished participation when meetings are attended. This pattern systematically removes the structure, accountability, and shared wisdom that these recovery communities uniquely provide. Common withdrawal patterns include attending recovery meetings much less frequently than previously established patterns, participating far less actively when meetings are attended, and feeling increasingly disconnected from the shared experience and common ground that these groups offer. Individuals may begin focusing primarily on perceived differences between themselves and others in recovery groups rather than recognizing shared experiences and mutual support opportunities. They often convince themselves that meetings are less necessary now that they've achieved some stability, failing to recognize that meetings often become more rather than less important as recovery progresses. This withdrawal removes regular exposure to recovery principles, disrupts vital connections with others on similar journeys, and eliminates the consistent accountability that regular meeting attendance naturally provides.
Risk Relationship Gravitation involves a magnetic pull toward relationships that align with, enable, or accommodate addictive patterns, representing both withdrawal from recovery-supportive relationships and simultaneous attraction to connections that make return to substance use more likely or acceptable. This dangerous pattern typically manifests as reconnecting with people from active addiction days who may still be using substances or living unstable lives, becoming interested in developing new relationships with people who actively use substances or have casual attitudes toward substance use, and systematically downplaying the recovery risks inherent in spending significant time with actively using individuals. People in this pattern often report feeling more authentic, understood, or accepted by individuals who aren't focused on recovery, and may actively seek relationships where their addiction history doesn't need to be acknowledged or discussed. This gravitation creates significant vulnerability by systematically surrounding oneself with relationships that normalize substance use and may directly or indirectly encourage relapse through modeling, availability, or social pressure to participate in substance-related activities.
Risk Environment Attraction involves the powerful draw toward physical locations and settings that are associated with past substance use or where substance use is prevalent, reflecting how physical environments can trigger intense associations and cravings through contextual memory and conditioned responses. This dimension often manifests as finding oneself inexplicably drawn to locations that were central to past substance use, deliberately spending time in environments where substance use is common or expected, or experiencing strong nostalgia about places that are connected to using days. Individuals may create elaborate justifications for visiting high-risk locations "just briefly" or for specific legitimate purposes, while convincing themselves that they have developed sufficient ability to safely navigate environments that are centered around substance availability and use. This pattern creates substantial vulnerability through repeated exposure to powerful environmental triggers that can activate well-established neural pathways for substance seeking, often overwhelming cognitive defenses and rational decision-making processes that might otherwise maintain recovery stability.
Selective Social Engagement represents perhaps the most subtle form of isolation, involving the maintenance of superficial recovery connections while systematically avoiding authentic intimacy or selectively engaging primarily with people who are less likely to challenge recovery drift or concerning patterns. This dimension reflects how significant isolation can occur even while appearing to maintain adequate social connection to outside observers. The pattern often appears as maintaining surface-level recovery connections that look appropriate but lack the depth necessary for genuine accountability, selectively engaging with people who are less likely to notice, question, or challenge concerning changes in recovery commitment or stability. Individuals may actively seek relationships that reinforce their current state rather than encouraging continued growth and recovery development, gravitate toward people who don't know their authentic recovery history and therefore can't recognize concerning changes, or systematically compartmentalize different social groups to maintain comfortable disconnection from those who might provide challenging but necessary feedback. This selective engagement creates vulnerability by preventing the authentic connection and meaningful accountability that are essential for sustainable recovery, while simultaneously creating the comfortable illusion of adequate social support that can mask the dangerous reality of increasing isolation from recovery-supportive relationships.
Understanding these social isolation dimensions is crucial because recovery is fundamentally a social process that requires ongoing connection with supportive relationships, communities, and professional resources. These isolation patterns often develop gradually and can feel natural or justified, while systematically removing the interpersonal foundation that recovery requires for long-term stability and success.
Inner Conflict- Conversation with Self
This self-assessment explores seven critical dimensions of inner conflict that can emerge during recovery, representing complex psychological battlegrounds where competing aspects of the self struggle for dominance over recovery decisions and commitment. These inner conflict dimensions are particularly challenging because they create internal division that can paralyze decision-making, undermine recovery practices, and generate profound psychological distress that threatens recovery stability.
Internal Dialogue Polarization involves experiencing distinct and powerfully competing internal "voices" or perspectives that represent fundamentally different orientations toward recovery and addiction. This dimension reflects the profound split between the recovering self that is oriented toward health, growth, and sobriety, and the addictive self that remains oriented toward return to substance use and the familiar patterns of addiction. Common manifestations include experiencing clearly competing internal voices with completely opposing recovery perspectives, feeling genuinely pulled between simultaneously wanting recovery and wanting to use substances again, and having thoughts that oscillate dramatically between strong commitment to sobriety and elaborate justifications for using. Individuals often notice clear distinctions between what they recognize as "sober thinking" and "addictive thinking," and may experience themselves as having multiple, contradictory identities related to addiction and recovery that feel equally real and compelling. This polarization creates profound internal distress because both perspectives can feel authentic and justified, often preceding behavioral inconsistency in recovery practices as the individual acts from whichever "self" is momentarily dominant.
Help-Seeking Paralysis represents one of the most dangerous aspects of inner conflict, involving the paradoxical experience of clearly recognizing the need for support while feeling completely unable to initiate contact with available recovery resources. This dimension reflects the powerful way that internal conflict can inhibit actions that the recovering self knows are necessary and beneficial for maintaining stability. The paralysis typically manifests as recognizing clearly that help is needed while feeling genuinely unable to reach out for that help, experiencing the simple act of making a phone call for support as disproportionately difficult or overwhelming, preparing mentally to contact recovery supports but consistently abandoning the attempt before completion. Individuals often describe feeling frozen between knowing that help is needed and being unable to ask for it, or experiencing a sense of being silenced by their own mind when trying to seek support. This phenomenon, sometimes described as the "too-heavy phone" syndrome, represents one of the most dangerous aspects of recovery because it prevents access to essential recovery resources precisely when they are most critically needed for preventing relapse or further deterioration.
Warning Recognition/Dismissal involves the simultaneous process of identifying important recovery warning signs while also generating reasons to minimize, rationalize, or completely ignore them. This dimension reflects how internal conflict can create a destructive pattern of acknowledging crucial recovery information and then systematically dismissing it before appropriate action can be taken. The pattern often appears as noticing concerning changes in recovery commitment or stability but then quickly minimizing their importance or significance, experiencing part of the self that clearly recognizes relapse warning signs while another part simultaneously dismisses these same signs as unimportant or temporary. Individuals may alternate between periods of clear recovery awareness where problems are obvious and periods of denial where the same problems seem insignificant, acknowledge concerning patterns internally but quickly generate elaborate reasons why there's no need to worry or take action. This creates a dangerous internal debate about whether legitimate recovery warning signs are actually significant enough to warrant intervention, preventing appropriate response to warning signs that could otherwise prompt protective recovery actions before more serious consequences develop.
Substance Use Fantasies involve detailed imaginative scenarios about returning to controlled, occasional, or "successful" substance use, typically emphasizing anticipated benefits while systematically minimizing or ignoring potential consequences. This dimension reflects how the addictive self maintains its influence and presence through selective and highly distorted thinking about substances and their effects. These fantasies typically include vivid imagining of scenarios where return to substance use occurs successfully, thinking about substances as potential "solutions" to current life difficulties or emotional challenges, and mentally rehearsing detailed plans for how using "just once" or in controlled ways might be manageable this time. Individuals often romanticize their past relationship with substances despite overwhelming evidence of negative consequences, and experience genuine nostalgia about the relief, pleasure, or escape that substances once seemed to provide. These fantasies create significant vulnerability by keeping substance use psychologically available as a viable option rather than maintaining it as completely off-limits, and by systematically strengthening neural pathways associated with substance-seeking behavior through repeated mental rehearsal and positive association.
Cure Delusion involves the development of beliefs that addiction has been permanently overcome or resolved, thereby eliminating the need for ongoing recovery practices, continued vigilance against relapse, or acknowledgment of addiction as a chronic condition requiring lifelong management. This dimension reflects a sophisticated form of denial that is specifically focused on rejecting the well-established understanding of addiction as a chronic condition. Common manifestations include entertaining thoughts about being fundamentally "different" from others with addiction in ways that make continued recovery practices unnecessary, believing that addiction has been permanently overcome through sufficient time in recovery or personal growth, thinking that adequate time in recovery eliminates ongoing vulnerability to relapse, developing elaborate theories about newfound ability to use substances moderately when such moderation was previously impossible, or considering oneself "graduated" from needing the ongoing recovery practices that created and maintain current stability. This delusion creates profound vulnerability by systematically undermining the ongoing practices, awareness, and vigilance that are necessary for sustained recovery from what is fundamentally a chronic condition requiring continuous management rather than a temporary problem that can be permanently solved.
Recovery Identity Ambivalence involves significant uncertainty, inconsistency, or conflict about identifying as a person in recovery from addiction, reflecting internal conflict about whether and how addiction and recovery should be integrated into fundamental self-concept and identity. This dimension often emerges after periods of recovery stability when individuals begin questioning their relationship to recovery identity and community. Signs of this ambivalence include questioning whether one truly belongs in recovery communities or shares enough common ground with others in recovery, feeling genuinely uncertain about whether addiction is or should be considered a fundamental part of personal identity, alternating between periods of embracing recovery-based identity and periods of rejecting or resenting it. Individuals may begin resisting recovery language and concepts that they previously accepted as accurate and helpful, or experience ongoing confusion about who they "really are" in relation to addiction and recovery. This ambivalence creates vulnerability by weakening commitment to recovery practices and community connections, which often depend on at least some level of identification with recovery principles, values, and shared experience with others who have similar struggles.
Behavioral Inconsistency involves significant and often dramatic variation in recovery practices and commitment based on which aspect of the self—recovering or addictive—is momentarily dominant in decision-making. This dimension represents how internal conflict directly impacts observable recovery behaviors and choices, creating unpredictable patterns that can confuse both the individual and their support systems. This inconsistency typically appears as recovery behaviors that fluctuate dramatically based on which internal "self" is dominant at any given time, making strong recovery commitments during periods when the recovering self is ascendant and then systematically undermining those same commitments when the addictive self gains influence. Individuals experience significant inconsistency between their stated recovery intentions and their actual actions, may maintain certain recovery practices conscientiously while simultaneously sabotaging others, and demonstrate levels of recovery engagement that vary widely without clear external reasons or explanations. This behavioral inconsistency creates substantial vulnerability by preventing the establishment of stable, reliable recovery practices and by creating a dangerous pattern where recovery commitment becomes contingent on fluctuating internal states rather than remaining consistent regardless of those temporary states.
Understanding these inner conflict dimensions is crucial because they represent the psychological battleground where recovery success or failure is often determined. These conflicts can create profound internal distress and behavioral inconsistency that threatens recovery stability, but recognition of these patterns enables the development of specific strategies for managing internal conflict and maintaining recovery commitment even when competing internal voices are present and active.
This self-assessment explores seven critical dimensions of crisis building that can emerge during recovery, representing progressive psychological and cognitive deterioration that systematically overwhelms coping resources and creates conditions where substance use begins to appear as a reasonable or necessary response to mounting difficulties. These crisis building dimensions are particularly dangerous because they often develop gradually and reinforce each other, creating cascading effects that can rapidly overwhelm even well-established recovery stability.
Problem Multiplication involves the overwhelming experience of challenges proliferating faster than they can be effectively addressed, creating a profound sense of being buried under accumulating difficulties that seem to grow exponentially rather than diminish through efforts to resolve them. This dimension reflects how addiction-affected thinking can transform ordinary life challenges into cascading crises through distorted perception and ineffective response patterns. Common manifestations include experiencing periods where problems genuinely seem to multiply faster than any reasonable person could address them, finding that sincere attempts to solve one issue often create or reveal additional unexpected problems, and discovering that problem-solving efforts feel counterproductive or even destructive. Individuals become genuinely overwhelmed by the sheer number of simultaneous challenges they're facing, and begin perceiving their various problems as interconnected in complex ways that make individual solutions seem impossible or futile. This multiplication creates profound vulnerability by systematically overwhelming available coping resources and creating the deeply held sense that problems are fundamentally unsolvable through conventional means, thereby setting the psychological stage for substance use to appear as a viable escape from an impossible situation.
Perspective Narrowing involves a progressive and dangerous constriction of cognitive flexibility, where thinking becomes increasingly rigid, black-and-white, and focused on immediate concerns while losing the ability to maintain broader perspective or access creative problem-solving resources. This dimension reflects how escalating stress affects fundamental cognitive function during crisis building periods. The narrowing typically manifests as thinking that becomes increasingly polarized during difficult periods, with complex situations reduced to simple either-or propositions that eliminate nuanced understanding. Individuals lose the ability to see the broader context of their challenges, becoming fixated on immediate problems at the expense of long-term considerations that might provide hope or alternative approaches. Their capacity for creative problem-solving diminishes significantly under pressure, and they struggle to remember or effectively apply past successful coping strategies that were previously accessible and effective. This narrowing creates profound vulnerability by systematically limiting access to the full range of cognitive resources that support effective coping and problem-solving, making substance use appear as one of the few remaining available options for managing overwhelming difficulties.
Emotional Escalation involves intensifying emotional distress that remains unexpressed, unprocessed, and unmanaged, creating mounting internal pressure that seeks relief through any available means. This dimension reflects how unaddressed emotions can build to overwhelming and potentially explosive levels during crisis progression. Signs of this dangerous escalation include experiencing intensifying emotional distress without sharing these feelings with others who might provide support or perspective, having emotional states that progressively deteriorate during problem periods rather than stabilizing through healthy processing. Individuals often attempt to suppress or escape uncomfortable emotions rather than working through them appropriately, engaging in various activities specifically designed to distract from emotional discomfort rather than address its sources, and cycling through increasingly negative emotional states without finding resolution or relief. This escalation creates significant vulnerability by generating intense emotional discomfort that, without healthy outlets and processing strategies, naturally seeks relief through any available means, including the temporary but familiar relief that substance use once provided.
Solution Dysfunction involves the counterproductive pattern of persisting with ineffective problem-solving approaches despite clear evidence of their failure, creating a cycle of diminishing returns, increasing frustration, and mounting desperation. This dimension reflects how addiction-affected thinking can create rigid, self-defeating response patterns that actually worsen rather than improve difficult situations. Common dysfunctional patterns include continuing to use strategies that accumulated evidence clearly shows aren't working, repeatedly applying the same ineffective approaches with unrealistic hopes of achieving different results, systematically rejecting suggestions from others about alternative approaches that might be more effective, becoming increasingly rigid rather than flexible in problem-solving approaches when flexibility is most needed, and engaging in behaviors that past experience has already demonstrated to be counterproductive or harmful. This dysfunction creates profound vulnerability by systematically exhausting available resources on approaches that don't work while problems continue to multiply and intensify, thereby increasing feelings of hopelessness, desperation, and the sense that conventional solutions are fundamentally inadequate for addressing current difficulties.
Planning Deterioration involves a progressive and dangerous decrease in the ability to organize, prioritize, and prepare for future events, creating an increasingly reactive rather than proactive stance toward life challenges that removes protective structure and foresight. This dimension reflects how crisis building systematically affects executive function and the capacity for forward-thinking that normally provides protection against escalating difficulties. Signs of this deterioration include significantly diminished ability to plan ahead as stress levels increase, becoming increasingly reactive rather than proactive in response to challenges, systematically abandoning previously established plans and structures when under pressure, focusing exclusively on immediate crises at the expense of preventative measures that could reduce future problems, and operating with a shortened time horizon that gives less consideration to future consequences of current decisions. This deterioration creates substantial vulnerability by removing the protective structure that effective planning normally provides, leaving individuals increasingly subjected to unmanaged crises that could have been prevented or minimized through appropriate foresight and preparation.
Perseveration and Rumination involve getting caught in repetitive, unproductive thought patterns that consume enormous amounts of mental energy without generating any useful solutions, creating an exhausting sense of being trapped in an unsolvable mental maze that demands escape. This dimension reflects how addiction-affected thinking can create profoundly distressing internal experiences that seem to require immediate relief through any available means. Common manifestations include thoughts that become increasingly repetitive and unproductive, consuming mental energy without moving toward resolution, experiencing a persistent sense of mental "spinning" or churning without any progress or relief, finding oneself completely unable to shift attention away from problems even briefly for mental rest or recovery. The thinking process itself creates a sense of being trapped in an inescapable cycle with no way out, and individuals find themselves ruminating obsessively on past failures rather than learning from them and moving forward constructively. This pattern creates dangerous vulnerability by systematically exhausting available mental resources while creating a desperate desire for relief from unrelenting internal distress that substance use once effectively provided.
Addictive Thinking Resurgence involves the progressive and increasingly powerful reemergence of thought patterns that justify, rationalize, or actively demand substance use, eventually presenting relapse not just as an available option but as a logical necessity for managing overwhelming circumstances. This dimension reflects how addiction can systematically hijack the cognitive process during periods of significant distress, gradually transforming perception until substance use appears reasonable or even essential. Signs of this dangerous resurgence include beginning to seriously consider substance use as a potential solution to current distress rather than recognizing it as a source of additional problems, experiencing the voice of addiction becoming progressively louder and more persuasive in internal dialogue, having intensifying internal debates between recovery-oriented and addiction-oriented perspectives where the addiction voice gains strength and credibility. The addictive thinking presents increasingly sophisticated and persuasive arguments for using substances, often framing use as temporary relief that will provide the clarity or energy needed to address overwhelming problems, and relapse begins to appear not just rational but necessary rather than recognizably destructive. This resurgence creates profound vulnerability by fundamentally transforming the perception of substance use from a destructive choice that creates additional problems into what appears to be a logical, reasonable, or even essential response to circumstances that seem truly overwhelming and unmanageable through conventional recovery means.
Understanding these crisis building dimensions is crucial because they represent progressive deterioration that can rapidly overwhelm even well-established recovery stability. These dimensions often develop gradually and reinforce each other in ways that create cascading effects, making early recognition and intervention essential for preventing the complete collapse of recovery defenses and the return to active addiction.
This document explores seven critical dimensions of immobilization that can emerge during recovery, representing a profound psychological state where individuals become essentially paralyzed in their ability to take constructive action despite being aware of what needs to be done. These immobilization dimensions are particularly dangerous because they create a self-perpetuating cycle where the inability to act leads to worsening circumstances, which further reinforces the sense of helplessness and paralysis, ultimately creating conditions where relapse may appear as the only viable escape from unbearable psychological states.
Problem Insolubility involves a fundamental cognitive shift where challenges are perceived as completely overwhelming, unsolvable, and beyond any possible influence or control, representing a mental state where individuals literally cannot perceive viable pathways forward regardless of what actions might potentially be taken. This dimension reflects a profound cognitive distortion where normal problem-solving capacity becomes completely inaccessible. Common manifestations include perceiving current problems as completely overwhelming and fundamentally unsolvable through any conceivable means, feeling genuinely trapped in circumstances that seem beyond any control or influence, and being unable to see any viable pathways forward regardless of potential actions that others might suggest or that were previously effective. Individuals experience their challenges as an endless, inescapable stream of difficulties without resolution, and develop the deep belief that any action they might take would be completely futile. This perception creates profound vulnerability by systematically undermining the fundamental motivation to take any recovery-supporting actions, as these actions appear completely pointless in the face of what seem to be insurmountable obstacles that cannot be influenced by human effort or intervention.
Motivational Depletion involves a profound exhaustion regarding recovery efforts, particularly emerging after periods where previous attempts at problem-solving have yielded limited or disappointing results, reflecting the emotional and energetic consequences of persistent struggle without perceived progress or meaningful improvement. This depletion typically manifests as feeling genuinely exhausted by repeatedly trying solutions that haven't worked or haven't provided the relief or progress that was hoped for, experiencing significantly diminished desire to continue working on recovery-related challenges, and seriously questioning whether continued effort is worth the enormous energy that recovery seems to require. Individuals develop profound weariness about recovery-related activities that once felt meaningful or hopeful, and find their motivation fluctuating between completely absent and minimal at best. This depletion creates dangerous vulnerability by systematically removing the essential energy needed to maintain recovery practices, especially during challenging periods when these practices are most necessary for preventing deterioration, creating a particularly cruel cycle where reduced motivation leads to reduced recovery activity, which often leads to worsening circumstances that require even more motivation to address effectively.
Action Inhibition represents perhaps the most frustrating dimension of immobilization, involving the complete inability to initiate or sustain necessary recovery-supporting behaviors despite clear awareness of their importance and potential effectiveness. This dimension reflects the profound gap that can develop between knowing what to do and being able to translate that knowledge into actual action. Signs of this debilitating inhibition include struggling to initiate even simple tasks that are known to be helpful and that were previously manageable, being completely unable to take actions that have been planned, committed to, or that others are depending on, experiencing a profound disconnection between knowing intellectually what needs to be done and being able to actually do it. Individuals find themselves postponing important recovery activities without clear or rational reasons, and may feel physically or mentally "frozen" when trying to begin tasks that should be straightforward. This inhibition creates significant vulnerability by preventing the implementation of recovery knowledge and strategies, leaving individuals aware of what they need to do but completely unable to execute these needed actions, creating a sense of being trapped by their own psychological paralysis.
Hopelessness Development involves the progressive and devastating loss of belief that positive change is possible, culminating in a psychological state where giving up entirely seems like the only rational response to persistent suffering and apparent lack of progress. This dimension reflects the emotional consequence of perceived permanent immobilization where improvement seems impossible. Common manifestations include feeling like giving up on recovery entirely because continued effort appears pointless, being unable to see any possibility for meaningful positive change in current circumstances or future prospects, believing deeply that the future contains only more struggle, difficulty, and disappointment without relief or improvement. Individuals experience a pervasive sense that things will never get better regardless of what they do, and have profound difficulty imagining any positive outcome to their current state or any reason to continue trying. This hopelessness creates profound vulnerability by systematically removing the expectation of improvement that normally sustains effort through difficult periods, making relapse appear as a reasonable alternative to continued suffering that seems both pointless and endless.
Negative Self-Perception involves developing a fundamentally distorted and harsh view of oneself as flawed, inadequate, or failing at recovery despite genuine efforts and often despite objective evidence of progress or growth. This dimension reflects how immobilization profoundly affects self-concept and self-evaluation in destructive ways. Typical manifestations include viewing oneself as fundamentally flawed or inadequate as a person, believing deeply that one is failing at recovery despite sincere efforts and often despite evidence to the contrary, experiencing intense and persistent self-criticism about recovery progress that goes far beyond realistic self-assessment. Individuals compare themselves unfavorably to others in recovery while ignoring differences in circumstances, resources, or starting points, and attribute their struggles entirely to personal defects rather than recognizing the role of circumstances, timing, or the inherent challenges of recovery itself. This negative self-perception creates dangerous vulnerability by generating intense shame that actively inhibits help-seeking behavior and reinforces isolation precisely when connection with others is most needed for breaking through the immobilization.
Facade Maintenance involves the exhausting effort of presenting a more positive recovery image to others than is authentically experienced, creating a dangerous gap between external presentation and internal reality that prevents access to needed support and understanding. This dimension reflects how shame and fear of judgment can create profound isolation even while appearing connected to recovery community and supports. Signs of this costly maintenance include presenting a significantly more positive recovery image to others than what is internally experienced, systematically withholding crucial information about true struggles from recovery supports who might be able to help, feeling completely unable to honestly share the immobilized state with others who care and want to support recovery efforts. Individuals often believe that others couldn't possibly understand their experience or would judge them harshly if they knew the full extent of their struggles, leading to maintaining an elaborate illusion of recovery progress while privately feeling completely stuck and hopeless. This facade creates profound vulnerability by preventing the authentic connection and support that could potentially help break through immobilization, leaving individuals to manage overwhelming experiences entirely alone despite appearing connected to others who want to help.
Escape Fantasies involve recurring and increasingly elaborate thoughts about geographical changes, magical interventions, or substance use as potential solutions to the pain and apparent hopelessness of immobilization. This dimension reflects the mind's desperate attempt to find relief from seemingly intolerable internal states when conventional solutions appear unavailable or ineffective. Common fantasies include believing that geographical changes—moving to different locations or completely changing life circumstances—could somehow solve internal struggles that are actually psychological rather than situational, hoping for magical or external intervention that would change circumstances without requiring personal action or effort, fantasizing about simply disappearing from current life and responsibilities to escape overwhelming demands and expectations. Perhaps most dangerously, individuals may increasingly view substances as viable means of escaping the immobilized state, and find significant mental energy being consumed by elaborate and unrealistic escape scenarios that become increasingly detailed and compelling. These fantasies create substantial vulnerability by directing valuable problem-solving energy toward completely unrealistic or actively harmful "solutions" rather than toward sustainable recovery strategies that might actually help, potentially culminating in relapse as what appears to be the ultimate and most accessible escape from unbearable psychological paralysis.
Understanding these immobilization dimensions is crucial because they represent a psychological state that can rapidly progress to relapse if not recognized and addressed through appropriate intervention. These dimensions often reinforce each other in ways that create deepening paralysis, making early recognition and intensive support essential for preventing complete recovery collapse during these vulnerable periods.
This self-assessment explores seven critical dimensions of painful problems that can emerge during recovery, representing distressing psychological and cognitive symptoms that create significant internal suffering and often drive individuals toward substance use as a means of relief. These dimensions reflect how recovery challenges can disrupt fundamental mental processes, creating cascading effects that undermine both daily functioning and recovery stability.
Cognitive Dysfunction involves significant difficulties with clear thinking, problem-solving, and logical reasoning that were previously manageable and automatic, representing a breakdown in basic cognitive processing that creates profound frustration and self-doubt. This dimension reflects how intense stress and recovery challenges can fundamentally affect the brain's ability to process information effectively. Common manifestations include struggling with clear thinking about relatively simple matters that should be straightforward, experiencing noticeable deterioration of problem-solving abilities during stressful periods when these skills are most needed, having difficulty organizing thoughts coherently enough to communicate effectively or make decisions, finding that the mind is functioning significantly less effectively than it has previously, and discovering that reasoning has become flawed or distorted in ways that lead to poor conclusions or decisions. This dysfunction creates substantial vulnerability by systematically undermining confidence in basic mental capabilities that are essential for navigating daily life, while simultaneously creating practical barriers to effectively addressing recovery challenges that require clear thinking and sound judgment.
Attention Disturbance involves profound difficulty regulating mental focus, with experiences that can range from racing, uncontrollable thoughts to unexpected mental blankness and complete inability to concentrate on necessary tasks. This dimension reflects how recovery challenges can severely disrupt the attentional control systems that are essential for effective functioning. The disturbance typically manifests as thoughts that race uncontrollably, making sustained focus on any single topic or task extremely difficult or impossible, experiencing unexpected periods where the mind goes completely blank during conversations or activities that require mental engagement, struggling persistently to maintain concentration on necessary tasks long enough to complete them effectively, having attention that shifts rapidly and unpredictably between different topics without allowing completion of any single focus area, and finding it genuinely difficult to focus long enough to complete even basic everyday activities that were previously automatic. This disturbance creates dangerous vulnerability by systematically interfering with the sustained attention that recovery practices require, while simultaneously creating intensely distressing internal experiences of mental chaos or emptiness that may prompt desperate attempts to find relief through substance use.
Memory Impairment involves unexpected and concerning difficulties with recall of recent events, conversations, commitments, and information that would normally be remembered without effort, representing a disruption in cognitive functions related to information retention and retrieval. This dimension reflects how recovery challenges can affect fundamental memory processes in ways that disrupt daily functioning and create additional stress. Signs of this impairment include forgetting important information that would normally be remembered easily, struggling to recall recent conversations or events that should be accessible in memory, missing appointments, commitments, or responsibilities due to genuine memory failures rather than avoidance, repeating questions or statements because previous discussions have been forgotten, and becoming confused about sequences of events or timeframes in ways that affect understanding of recent experiences. This memory impairment creates significant vulnerability by disrupting normal daily functioning, systematically undermining self-trust and confidence in basic mental capabilities, and potentially creating embarrassing or problematic situations that increase stress levels and compound existing recovery challenges.
Emotional Volatility involves experiencing persistent restlessness, irritability, general discontent, and rapid, intense emotional shifts that seem completely disproportionate to triggering events, reflecting how recovery challenges can severely disrupt normal emotional regulation systems. Common volatility patterns include experiencing chronic restlessness, irritability, and general discontent that colors most daily experiences negatively, having emotional reactions that seem dramatically disproportionate to the events that triggered them, experiencing rapid shifts between different emotional states that create internal chaos and confusion, having intense anger arise suddenly without adequate provocation or warning, and experiencing mood changes that occur without any clear external causes or explanations. This volatility creates substantial vulnerability by generating intense and persistent emotional discomfort that becomes difficult to tolerate, creating significant difficulties in relationships with family, friends, and recovery supports who may not understand these emotional fluctuations, and potentially triggering substance use as a desperate attempt at emotional regulation when healthy coping strategies seem inadequate for managing the intensity of emotional experience.
Interpersonal Friction involves increased conflicts, irritation specifically directed at close relationships, and mounting frustration with others for their perceived lack of understanding or adequate support during difficult periods. This dimension reflects how internal distress often manifests in relational difficulties that can damage essential recovery supports. Typical friction patterns include directing anger, irritation, or criticism disproportionately toward those who are closest and most supportive, becoming increasingly frustrated with others for not understanding the depth of current struggles or not providing the type or amount of help that feels needed, perceiving others as deliberately unhelpful, obstructive, or unsympathetic when they may actually be trying to be supportive, engaging in conflicts and arguments more frequently than usual over issues that might normally be manageable, and becoming easily annoyed by others' normal behaviors, comments, or attempts to help that would typically be appreciated or at least tolerated. This friction creates dangerous vulnerability by systematically damaging the essential recovery relationships and support systems that are most crucial for maintaining stability, increasing isolation precisely when connection is most needed, and generating additional interpersonal stressors that compound existing challenges and create new problems that require energy and attention to resolve.
Emotional Dysregulation represents a more severe form of emotional disruption involving oscillation between emotional extremes—both overreaction and complete numbness—coupled with counterproductive attempts to suppress uncomfortable feelings rather than processing them appropriately. This dimension reflects more profound disruption of emotional management systems that can create cascading psychological problems. Signs of this dysregulation include oscillating unpredictably between emotional overreaction where feelings seem overwhelming and uncontrollable, and emotional numbness where normal feelings seem completely inaccessible, experiencing emotions as genuinely overwhelming and uncontrollable in ways that feel frightening or foreign, feeling emotionally disconnected from people and situations that are normally important and meaningful, making persistent attempts to suppress or ignore uncomfortable emotions rather than working through them appropriately, and experiencing emotional states that feel completely foreign or unlike one's normal emotional self. This dysregulation creates profound vulnerability by generating intense internal distress while simultaneously undermining the healthy emotional processing skills that are essential for recovery, potentially creating a self-perpetuating cycle where emotional dysregulation leads to poor coping attempts, which then lead to even greater dysregulation.
Self-Trust Deterioration involves progressively questioning one's own perceptions, feelings, and decision-making capabilities, sometimes escalating to genuine fears of "going crazy" and deliberate attempts to override natural intuitive responses that might actually be helpful. This dimension reflects how recovery challenges can fundamentally undermine trust in oneself and one's ability to navigate life effectively. Common manifestations include persistently questioning whether current perceptions and feelings are accurate or trustworthy, developing serious doubts about the ability to navigate everyday challenges that were previously manageable, experiencing genuine fear of "going crazy" or losing mental stability entirely, making decisions that are later recognized as poor or impulsive but that seemed reasonable at the time, and actively mistrusting emotional responses while trying to override them rather than using them as valuable information. This deterioration creates substantial vulnerability by systematically undermining the self-trust that is absolutely necessary for effective recovery navigation, potentially leading to poor decisions that create additional problems and complications, and making it difficult to rely on internal wisdom and intuition that might otherwise guide appropriate recovery choices.
Understanding these painful problem dimensions is crucial because they represent genuine psychological suffering that creates powerful motivation to find relief through any available means, including substance use. These symptoms often feel overwhelming and unmanageable through conventional recovery strategies, making professional intervention and intensive support essential for addressing the underlying issues while maintaining recovery stability during these challenging periods.
This self-assessment explores twelve critical dimensions of addictive thinking that represent sophisticated psychological mechanisms used to justify, rationalize, and ultimately enable return to substance use during recovery. These dimensions illustrate how addiction fundamentally hijacks cognitive processes, creating elaborate mental frameworks that make relapse appear reasonable, necessary, or inevitable while systematically dismantling the psychological foundation that recovery requires.
Value Violation involves engaging in behaviors that directly contradict personal values and principles, leading to profound diminishment of self-respect and internal psychological dissonance that creates vulnerability to further moral compromise. This dimension reflects how addictive thinking creates increasingly sophisticated justification for actions that the person previously considered completely unacceptable or wrong. Common manifestations include engaging in behaviors that clearly contradict deeply held personal values, making choices that are known to cause harm to oneself or loved ones while finding ways to rationalize these choices, experiencing steadily decreasing self-respect due to one's own actions and decisions, doing things that the "recovering self" would strongly disapprove of while finding mental justification for these actions, and developing an increasingly wide gap between stated values and actual behaviors. This violation creates substantial vulnerability by systematically undermining the personal integrity and moral foundation that are necessary for sustainable recovery, while generating shame and self-disgust that can fuel further addictive thinking as the person seeks relief from the painful awareness of their own moral compromise.
Treatment Avoidance involves finding increasingly elaborate reasons to disengage from therapeutic supports and recovery communities that previously provided essential anchoring for recovery stability. This dimension reflects how addictive thinking creates systematic justification for disconnecting from the very resources that are most capable of challenging distorted thinking and providing reality-based perspective. This avoidance typically manifests as finding reasonable-sounding excuses to miss therapy or counseling appointments that were previously prioritized, systematically decreasing attendance at recovery meetings or support groups that once provided structure and accountability, convincing oneself that effective communication with treatment providers is impossible or pointless, developing doubts about whether providers or group members can truly understand one's unique situation or struggles, and questioning the fundamental value or effectiveness of professional help and recovery support despite previous evidence of their benefit. This avoidance creates dangerous vulnerability by systematically removing structured supports precisely when they are most needed to counter returning addictive thinking patterns, leaving the individual without external reality-testing or professional guidance during increasingly vulnerable periods.
Relational Disconnection involves actively pushing away potential supports through anger, criticism, or systematic fault-finding, often motivated by underlying fear of judgment, vulnerability, or having distorted thinking challenged by people who care. This dimension reflects how addictive thinking deliberately sabotages essential relationships that could otherwise provide perspective and challenge distorted perceptions. Signs of this disconnection include systematically distancing from supportive people through expressions of anger, criticism, or fault-finding that may be unfair or exaggerated, using others' perceived shortcomings as justification for disconnection even when these shortcomings are minor or normal human flaws, rejecting genuine offers of potential support due to fear of judgment or having to be vulnerable about current struggles, actively pushing away people who might challenge current thinking patterns or decisions, and perceiving others as fundamentally unable or unwilling to provide meaningful help despite evidence to the contrary. This disconnection creates substantial vulnerability by systematically isolating the individual from perspectives that could effectively counter addictive thinking, while simultaneously creating additional relational problems and conflicts that intensify distress and provide further justification for self-destructive choices.
Isolation Progression represents the gradual but increasingly complete withdrawal from social connections and recovery community, eventually creating a psychological state where reaching out for help feels genuinely impossible despite desperate need for connection. This dimension reflects the cumulative impact of relational disconnection over time, creating progressive social isolation that becomes self-reinforcing. This progression typically appears as gradually withdrawing from social connections and recovery community involvement that once provided meaning and support, experiencing increasing aloneness that is primarily due to one's own choices rather than external circumstances, perceiving a steadily shrinking circle of available support even when support may actually be available, feeling genuinely unable to reach out even to people who were once close and supportive, and developing the belief that there is literally no one left to turn to for meaningful help or understanding. This isolation creates profound vulnerability by systematically removing external reality-testing and support resources, leaving the individual completely alone with increasingly distorted thinking patterns that go unchallenged by outside perspective or caring feedback.
Self-Pity Indulgence involves focusing obsessively on the unique difficulty of one's circumstances, perceiving oneself primarily as a victim of forces beyond control, and using expressions of suffering to gain attention or avoid taking responsibility for recovery-related actions. This dimension reflects how addictive thinking systematically distorts perception toward a self-centered victim stance that justifies giving up on recovery efforts. Common manifestations include focusing extensively on how uniquely difficult one's circumstances are compared to others, using expressions of suffering strategically to gain attention, sympathy, or to avoid taking responsibility for recovery-related choices, comparing one's situation unfavorably to others while ignoring advantages or resources that may be available, dwelling persistently on perceived unfairness or hardships while minimizing personal agency or capability, and viewing oneself primarily as a victim of circumstances that are completely beyond personal control or influence. This indulgence creates dangerous vulnerability by providing elaborate justification for disengagement from recovery efforts and potentially setting the psychological stage for substance use as "deserved" relief from perceived suffering that seems both unique and insurmountable.
Dishonesty Patterns involve engaging in systematic deception despite conscious awareness of problematic behavior, creating elaborate justifications and rationalizations, and maintaining deliberate denial about the seriousness of the current situation. This dimension reflects how addictive thinking fundamentally undermines the rigorous honesty that is essential for recovery success. Signs of these patterns include engaging in deliberate deception about thoughts, feelings, or behaviors despite being aware that these patterns are problematic, systematically rationalizing or minimizing concerning actions or thoughts to avoid facing their true significance, creating increasingly elaborate explanations to justify questionable choices or decisions that would normally be recognized as harmful, presenting a deliberately false image of recovery stability and progress to others who care, and maintaining active denial about the seriousness of the current psychological and spiritual situation despite mounting evidence of deterioration. These patterns create substantial vulnerability by preventing accurate self-assessment and appropriate intervention from others, allowing addictive thinking to progress unchallenged by reality-based feedback or accountability.
Shame Escalation involves experiencing steadily increasing shame about behaviors and choices, becoming psychologically paralyzed by guilt, and hiding one's authentic self due to fear of others' reactions and judgment. This dimension reflects how addictive thinking creates a vicious cycle where shame prevents the healing actions that could reduce shame, thereby increasing shame further in a self-perpetuating spiral. Common manifestations include experiencing intensifying shame about current behaviors, choices, and the overall direction of recovery, feeling genuinely unable to take constructive action despite knowing intellectually what needs to be done, becoming increasingly paralyzed by guilt about the current state of recovery and life circumstances, systematically hiding one's true self, thoughts, and struggles due to intense fear of others' reactions, and developing the belief that one has fallen too far from previous recovery progress to ever regain that ground. This escalation creates profound vulnerability by generating intense emotional pain that can seem escapable only through substance use, while simultaneously preventing the honest disclosure and vulnerability that could interrupt the shame cycle and enable appropriate help and support.
Emotional Imprisonment involves feeling completely trapped by overwhelming emotional states and developing the belief that effective emotional management is permanently impossible or beyond one's capability. This dimension reflects how addictive thinking catastrophizes emotional experiences and systematically removes hope for improvement or effective coping. Signs of this imprisonment include feeling genuinely trapped by overwhelming emotional states that seem to have no resolution or relief, believing deeply that one will never be able to manage emotions effectively again despite previous evidence of emotional growth in recovery, experiencing current emotional challenges in recovery as worse than the emotional state during active addiction, seeing absolutely no end to current emotional suffering regardless of what actions might be taken, and using emotional pain as primary justification for giving up on recovery efforts entirely. This imprisonment creates dangerous vulnerability by making substance use appear as the only viable escape from intolerable emotional states, despite clear evidence of previous emotional management successes achieved during recovery.
Help Rejection involves developing the belief that others cannot provide meaningful assistance, systematically dismissing suggestions or support from people who care, and developing a deep conviction that one's situation is uniquely beyond anyone's ability to help or understand. This dimension reflects how addictive thinking creates isolation by systematically undermining faith in potential solutions or external assistance. Common manifestations include no longer believing that other people, regardless of their qualifications or caring, can provide genuine help, automatically dismissing suggestions or support from recovery allies and professionals without fair consideration, developing a strong conviction that one's situation is completely beyond anyone's ability to assist or understand, perceiving previous sources of support as having suddenly become ineffective or inadequate, and rejecting offered help based on perceived inadequacy rather than actual experience of trying the suggested approaches. This rejection creates substantial vulnerability by systematically cutting off potential solutions and reinforcing the dangerous belief that one's condition is uniquely hopeless and beyond any possible remedy or intervention.
Control Delusion involves repeatedly trying to regain control using the same failed approaches, experiencing accelerating loss of control despite increasing efforts, and refusing to accept powerlessness despite mounting evidence that control attempts are counterproductive. This dimension reflects how addictive thinking prioritizes the comforting illusion of control over the effective surrender that recovery requires. Signs of this delusion include repeatedly trying to regain control over thoughts, emotions, or circumstances using the same approaches that have already proven ineffective, experiencing accelerating loss of control despite increasingly frantic efforts to manage unmanageable situations, refusing to accept powerlessness over addiction and its effects despite overwhelming evidence that control attempts have failed, believing that one simply needs to try harder to manage situations that are fundamentally unmanageable through personal effort alone, and experiencing growing frustration and desperation at the inability to control life circumstances through willpower or determination. This delusion creates dangerous vulnerability by systematically exhausting physical, emotional, and spiritual resources on ineffective control efforts while preventing the surrender to powerlessness that is necessary for genuine recovery progress.
Futility Perception involves experiencing recovery efforts as completely meaningless regardless of what actions are taken, feeling trapped in repetitive patterns without any possibility of progress, and believing that no amount of work or effort will improve the recovery situation. This dimension reflects how addictive thinking creates a sense of permanent stagnation and hopelessness regardless of actual circumstances or available resources. Common manifestations include experiencing all recovery efforts as fundamentally meaningless regardless of what specific actions are taken, feeling trapped in repetitive patterns and cycles without any genuine progress or forward movement, perceiving all efforts, past and present, as wasted or completely ineffective in creating positive change, believing deeply that no amount of work, effort, or commitment will improve the overall recovery situation, and experiencing recovery itself as a hopeless circular pattern that leads nowhere productive or meaningful. This perception creates profound vulnerability by systematically undermining motivation for continued recovery efforts and making substance use appear as a reasonable alternative to seemingly permanent futility and meaninglessness.
Option Narrowing represents perhaps the most dangerous dimension, involving perceiving available choices as increasingly limited, developing rigid black-and-white thinking about possible outcomes, and ultimately seeing only catastrophic options—insanity, suicide, or relapse—as potential endpoints to current suffering. This dimension reflects how addictive thinking progressively eliminates perception of viable alternatives until relapse appears inevitable. Signs of this narrowing include perceiving available life choices as increasingly limited despite potential options that may actually exist, believing that one faces only catastrophic options for the future with no middle ground or gradual improvement possible, developing rigid black-and-white thinking about possible outcomes that eliminates nuanced or partial solutions, experiencing mounting hopelessness about finding any viable solutions to current difficulties, and seeing only insanity, suicide, or relapse as the potential endpoints to current psychological suffering. This narrowing creates ultimate vulnerability by making relapse appear not just reasonable but inevitable rather than recognizing it as one choice among many available alternatives, potentially creating a self-fulfilling prophecy where the perceived lack of options leads directly to actual relapse.
Understanding these addictive thinking dimensions is crucial because they represent the sophisticated cognitive framework that typically precedes and justifies relapse, often developing gradually over time in ways that feel entirely logical and justified to the person experiencing them. Recognition of these patterns by individuals in recovery, their support systems, and treatment professionals can enable intervention before these thinking patterns translate into actual substance use.
This self-assessment explores twelve critical dimensions of high-risk thinking and behavior that represent the final stages before relapse, where individuals have moved beyond general vulnerability into active consideration and preparation for substance use. These dimensions illustrate how addiction systematically dismantles recovery defenses through sophisticated cognitive distortions, behavioral changes, and environmental manipulations that make relapse appear not just reasonable but inevitable.
Relief-Seeking Rationalization involves the fundamental reframing of substances from recognized sources of problems to perceived solutions for current difficulties, representing a complete cognitive reversal of the understanding that originally motivated recovery. This dimension reflects how addictive thinking positions substances as necessary medicine rather than destructive agents. Common manifestations include thinking that substances would provide genuine relief from current emotional pain rather than creating additional suffering, believing that using would actually solve problems currently being faced rather than compounding them exponentially, seeing substances as legitimate medicine for psychological suffering rather than recognizing them as sources of greater distress, romanticizing the immediate temporary effects of substances while systematically minimizing or forgetting the devastating consequences that inevitably follow, and experiencing current emotional states as genuinely unbearable without chemical relief despite evidence of previous emotional management success. This rationalization creates profound vulnerability by fundamentally reframing substances as therapeutic necessities rather than recognizing them as the source of greater suffering, making use appear as medical treatment rather than self-destructive behavior.
Comparative Reasoning involves conducting a distorted cost-benefit analysis that systematically weighs current distress against the perceived relief of substance use, consistently concluding that using "couldn't make things worse" or seems preferable to available alternatives. This dimension reflects how addictive thinking hijacks rational decision-making processes to favor immediate relief over long-term consequences. Signs of this reasoning include thinking that substances genuinely seem better than all perceived alternatives currently available, believing that relapse "couldn't possibly make things worse" than the current situation despite overwhelming evidence to the contrary, comparing current distress unfavorably to the temporary and illusory relief that substance use once appeared to provide, seeing using as clearly preferable to continuing to experience current emotions or circumstances, and telling oneself that since the situation seems hopeless anyway, using substances won't matter or make any meaningful difference. This reasoning creates dangerous vulnerability by making substance use appear completely rational through deliberately deceptive comparisons that systematically minimize devastating negative consequences while grossly exaggerating potential benefits that are temporary and ultimately destructive.
Control Illusion involves convincing oneself that controlled, moderate substance use would somehow be possible this time despite extensive previous evidence demonstrating complete powerlessness over substances. This dimension reflects how addictive thinking selectively ignores or reinterprets the overwhelming reality of powerlessness that was clearly demonstrated by past experience. Common illusions include convincing oneself that controlled use is genuinely possible despite a clear history of losing control, believing that recovery knowledge and experience somehow enable moderate use that was previously impossible, thinking that previous addiction problems were primarily circumstantial rather than reflecting a fundamental inability to control substance use, creating detailed and elaborate scenarios about how controlled use could work this time, and selectively remembering brief periods of apparent controlled use while systematically forgetting the inevitable loss of control that followed. This illusion creates substantial vulnerability by fundamentally undermining the core recovery concept of powerlessness over substances and creating dangerous false confidence in an ability to manage what extensive experience has proven to be completely unmanageable.
Secrecy Justification involves developing the belief that hidden substance use somehow "doesn't count" or would have significantly fewer consequences than disclosed use, representing an attempt to separate behavior from accountability and consequences. This dimension reflects how addictive thinking creates artificial partitions between actions and their natural results. Signs of this justification include believing that undisclosed substance use "doesn't really count" as relapse or doesn't represent the same level of recovery failure, making detailed plans to hide evidence of substance use from family, friends, and recovery supports, thinking that secret use would somehow have fewer consequences than open use despite the additional problems that secrecy creates, believing that recovery appearances could be maintained indefinitely while secretly using substances, and minimizing the fundamental significance of hiding behaviors that directly contradict recovery principles. This justification creates dangerous vulnerability by systematically removing the protective factor of accountability and transparency while creating a deceptive partition between public recovery identity and private addictive behavior that inevitably leads to escalating problems.
Recovery Restart Fantasy involves the comforting but completely unrealistic belief that one could simply get sober again after temporary substance use, systematically minimizing the enormous difficulty of the previous recovery journey while overestimating one's ability to stop using at will. This dimension reflects how addictive thinking creates a dangerous illusion of easy reversibility. Common fantasies include telling oneself confidently that one could simply get sober again after temporary or "controlled" use, believing that current recovery knowledge somehow guarantees the ability to stop using again despite evidence that knowledge alone is insufficient, thinking that one could use substances "just until" current pain or problems subside and then easily return to sobriety, viewing potential relapse as merely a temporary detour rather than recognizing it as dangerous regression that could lead to devastating consequences, and systematically minimizing the enormous difficulty, time, and effort that the previous path to sobriety actually required. This fantasy creates profound vulnerability by removing healthy fear of consequences through the false promise that any damage from relapse could be easily and quickly undone, making the decision to use seem low-risk and completely reversible when the reality is often quite different.
Support Network Disconnection involves systematically withdrawing from recovery-supportive relationships, hiding true thoughts and feelings from people who could provide help, and becoming increasingly unreachable to individuals who understand one's recovery history and could provide intervention. This dimension reflects how addictive thinking deliberately removes protective connections that could challenge distorted thinking or provide alternative perspectives. Signs of disconnection include deliberately withdrawing from recovery-supportive relationships that previously provided stability and accountability, systematically hiding true thoughts, feelings, and struggles from recovery supports who could potentially provide help or intervention, becoming increasingly unreachable to people who know one's recovery well and could recognize concerning changes, creating elaborate excuses to avoid recovery meetings, connections, or activities that might provide reality-testing, and developing the belief that no one would truly understand the current situation or be able to provide meaningful assistance. This disconnection creates substantial vulnerability by systematically eliminating accountability, reality-testing, and support precisely when these resources are most desperately needed to counter increasingly distorted addictive thinking.
High-Risk Association involves actively seeking relationships and connections with people who would support, enable, or normalize substance use while simultaneously distancing from individuals who are committed to recovery principles. This dimension reflects how addictive thinking systematically draws individuals toward influences that facilitate relapse while avoiding influences that might challenge addictive decisions. Common patterns include deliberately spending time with people who actively use substances and would not challenge or discourage relapse, actively seeking new relationships with people who would support or enable substance use rather than recovery, maintaining or reestablishing connections with former using associates and networks, gravitating toward people who question the necessity of recovery or encourage "loosening up" recovery standards, and systematically distancing from people who are firmly committed to recovery and might provide challenging but helpful feedback. This association creates dangerous vulnerability by surrounding oneself with influences that normalize substance use and systematically undermine recovery commitment, while simultaneously reducing exposure to recovery-affirming perspectives that could provide alternative viewpoints during vulnerable periods.
Environmental Testing involves deliberately placing oneself in situations where substances are present or available, testing resistance through exposure to powerful triggers, and systematically removing previously established environmental safeguards that protected recovery stability. This dimension reflects how addictive thinking creates opportunities for relapse through deliberate environmental exposure. Signs of testing include deliberately placing oneself in locations or situations where substances are present and available, actively testing one's ability to resist by repeatedly exposing oneself to known triggers and high-risk situations, visiting locations that are strongly associated with past substance use and that carry powerful environmental cues, systematically removing environmental safeguards and protective measures that were previously established to maintain recovery, and creating or allowing easy access to substances through environmental choices or relationships. This testing creates substantial vulnerability by repeatedly activating powerful conditioned responses and cravings while normalizing high-risk exposure, simultaneously demonstrating a willingness to compromise previously established boundaries that were designed to protect recovery stability.
Help Rejection involves developing the firm belief that no one could possibly help with current struggles, making advance decisions not to reach out for support before potential relapse, and rejecting the fundamental idea that external support could provide viable alternatives to substance use. This dimension reflects how addictive thinking systematically eliminates potential sources of intervention that might prevent relapse. Common manifestations include believing deeply that no one could genuinely help with current struggles or provide meaningful assistance, making deliberate advance decisions not to reach out for help before potential relapse occurs, convincing oneself that others' guidance, support, or intervention wouldn't change the current situation or provide viable alternatives, rejecting the basic idea that support systems could provide realistic alternatives to using substances for managing current difficulties, and believing that one's mind is already completely made up about using substances regardless of what others might say or offer. This rejection creates dangerous vulnerability by systematically closing off avenues for perspective, support, and intervention that might otherwise prevent relapse, leaving individuals completely alone with increasingly distorted thinking patterns that go unchallenged by external reality or caring feedback.
Surrender to Inevitability involves developing a fatalistic perspective where relapse feels completely predetermined regardless of any actions that might be taken, experiencing complete powerlessness to prevent eventual substance use, and viewing the entire situation through a lens of unavoidable failure. This dimension reflects how addictive thinking creates a self-defeating fatalistic perspective that systematically undermines personal agency and choice. Signs of surrender include feeling deeply that relapse is completely inevitable regardless of what actions might be taken to prevent it, experiencing profound powerlessness to prevent eventual substance use despite having options that haven't been fully explored, viewing the current situation exclusively through a lens of predetermined failure rather than recognizing available choices, believing fundamentally that one is simply delaying an unavoidable relapse rather than actively choosing recovery on a daily basis, and feeling like going through recovery motions while internally waiting for the inevitable moment of substance use. This surrender creates profound vulnerability by systematically undermining the essential belief in choice and personal agency that recovery requires, making relapse appear as destiny or fate rather than recognizing it as a decision, thus reducing motivation to resist or seek alternatives.
Last Threshold Awareness involves recognizing that relapse risk has become imminent, sensing that one is standing at the very edge of actual substance use, and often experiencing a deceptive and dangerous sense of calm about impending use. This dimension reflects the final cognitive stage before actual physical relapse occurs. Common experiences include clearly recognizing that risk of relapse has become imminent and immediate rather than theoretical, sensing that one is standing directly at the edge of actual substance use with only a final decision remaining, experiencing a dangerous sense of calm or certainty about impending use that can mask the gravity of the situation, making increasingly specific and detailed plans for exactly how and when substance use will occur, and feeling positioned at the final moment of choice before actual using begins. This awareness creates ultimate vulnerability by normalizing the immediate proximity to substance use and often involves a deceptive sense of calm or resignation that can mask the extreme gravity of the situation until actual use occurs, representing the last opportunity for intervention before relapse becomes behavioral reality.
Recovery Abandonment represents the final cognitive surrender where individuals completely reject recovery principles, discard their identity as people in recovery, and conclude that sobriety is not a viable long-term solution for their lives. This dimension reflects the ultimate surrender of recovery identity and commitment before relapse occurs. Signs of abandonment include believing fundamentally that recovery principles no longer apply to current circumstances or needs, actively rejecting previously accepted and helpful aspects of the recovery program, deciding that recovery has become completely irrelevant to current life situations and challenges, concluding definitively that sobriety is not a viable long-term solution despite evidence of its previous benefits, and completely discarding identification as a person in recovery along with the values and commitments that identity entailed. This abandonment creates ultimate vulnerability by removing the final cognitive barriers to relapse through the complete rejection of recovery as a viable life path, making substance use appear not just likely but entirely appropriate and justified given the fundamental abandonment of recovery identity and principles.
Understanding these high-risk dimensions is crucial because they represent the final stages before actual substance use occurs, where thinking and behavior have progressed beyond general vulnerability into active preparation for relapse. These patterns often develop rapidly once they begin and require immediate intensive intervention to prevent progression to actual substance use.