Mastering Clinical Supervision: Essential Competencies for Effective Leadership in Addiction Treatment
The field of substance use disorder treatment faces a critical challenge that threatens the quality and effectiveness of patient care: the persistent gap between clinical expertise and supervisory competence. This workbook addresses the systemic issue arising from promoting clinicians to supervisory roles based primarily on clinical experience or organizational necessity rather than demonstrated leadership capabilities. The practice of elevating practitioners to leadership positions without adequate preparation or aptitude for supervision creates cascading effects that impact team dynamics, patient care quality, and organizational effectiveness.
A fundamental misconception in the field is the assumption that clinical expertise naturally translates to supervisory competence. Research indicates that the skill sets required for effective clinical practice often differ substantially from those needed for successful leadership and supervision. Clinical supervisors in substance use disorder treatment must navigate complex intersections of clinical oversight, administrative responsibility, and leadership dynamics, requiring a sophisticated blend of competencies that extends far beyond clinical knowledge alone.
This workbook provides comprehensive self-assessment tools designed to help current and aspiring clinical supervisors identify their strengths and development areas across the critical competencies required for supervisory excellence. Each assessment follows a structured format that explores both challenges and competencies, providing scoring systems, detailed explanations, self-reflection questions, personalized development mapping, and action planning frameworks.
The Accidental Supervisor: A Clinical Leader's Journey Through the Looking Glass
A Narrative from the Trenches of Substance Use Disorder Treatment
So there I was, minding my own business, being perfectly competent at helping people recover from addiction, when someone in a suit decided I'd make an excellent supervisor. Apparently, the logic went something like this: "He's good with patients and hasn't quit yet—clearly management material!" Because nothing says "leadership potential" quite like the ability to tolerate our organizational dysfunction while maintaining therapeutic rapport with someone experiencing withdrawal.
The Great Awakening: When Clinical Skills Meet Management Reality
The first day in my new role, I discovered that my extensive training in motivational interviewing had not, in fact, prepared me to motivate Terry from accounting to process our invoices correctly. Nor did my expertise in cognitive-behavioral therapy translate seamlessly to helping Brad and Jennifer resolve their ongoing feud about who forgot to order coffee supplies. Turns out, "How does that make you feel?" isn't actually the solution to every workplace problem. Who knew?
I quickly learned that Clinical Leadership Foundation isn't just about being really good at addiction counseling while occasionally checking in on other people doing addiction counseling. It's about maintaining clinical credibility (so staff don't think you've "gone to the dark side") while simultaneously proving to organizational leadership that you understand spreadsheets and strategic planning. It's like being bilingual, except one language is "evidence-based practice" and the other is "synergistic operational efficiency metrics." Most days I feel like I need a translator.
The Team Building Adventure: Herding Cats Who Specialize in Trauma
Team Building and Culture Development sounded so straightforward in theory. Create a positive work environment! Foster collaboration! Build morale! What they didn't mention is that I'd be doing this with a group of highly trained professionals who chose to work in addiction treatment—which, let's be honest, doesn't exactly attract people who shy away from dysfunction or avoid challenging situations.
My team includes Sarah, who's been here since the building was constructed and has strong opinions about every change made since 1987; Marcus, the brilliant new grad who's convinced he can revolutionize addiction treatment with an app; Janet, who somehow maintains perfect documentation while everyone else scrambles to meet deadlines; and Kevin, whose approach to conflict resolution is to eat lunch in his car until problems resolve themselves. Building team cohesion among this crew is like trying to create a synchronized swimming routine with dolphins, a sea turtle, a shark, and a very anxious pufferfish.
Communication: The Art of Speaking Multiple Languages Simultaneously
Then there's Communication and Conflict Resolution—the competency that makes or breaks everything else. I've discovered that being a supervisor means becoming a translator between multiple universes that coexist in the same building. When I talk to clinical staff, I need to speak "patient-centered care with inadequate resources." When I talk to administration, it's "outcome metrics with cost containment." When I talk to regulatory inspectors, it's "complete compliance despite the chaos." And when I talk to patients' families, it's "we're absolutely doing everything possible while managing seventeen different crises simultaneously."
The really fun part is having difficult conversations about performance while maintaining therapeutic rapport. Try explaining to someone that their charting needs improvement without triggering their abandonment issues. Or mediating between two clinicians who both think the other one "doesn't understand trauma-informed care" when really they just have different opinions about whether playing music during group therapy is healing or disruptive.
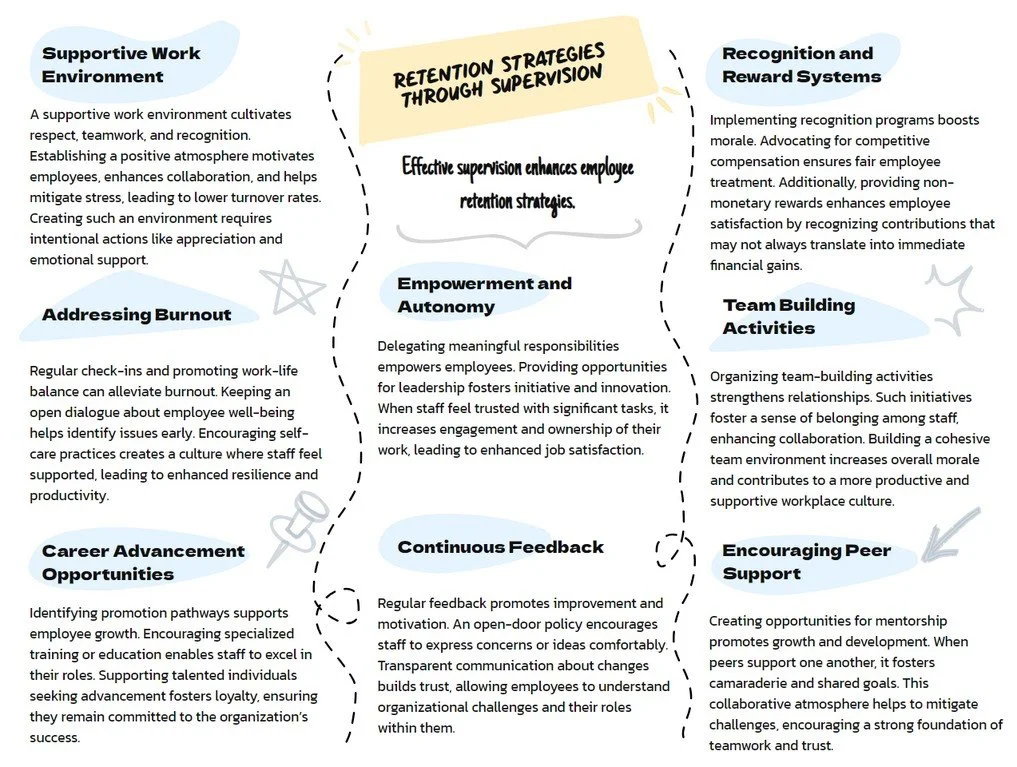
The Retention Puzzle: Making People Want to Stay in Wonderland
Retention Strategies became my obsession after watching our fourth excellent counselor leave for a job that pays $2 more per hour and includes free gym membership. Apparently, my heartfelt speeches about "making a difference" and "being part of something meaningful" lose their motivational power when people can't afford groceries or haven't had a vacation in three years.
I learned that creating a "supportive work environment" means more than just saying "we're all family here" while expecting everyone to work overtime during their family emergencies. It means actually preventing burnout instead of just acknowledging it exists. It means creating career advancement opportunities that don't require waiting for someone to retire or, let's be honest, have a breakdown. It means recognizing achievements in ways that feel authentic rather than like participation trophies handed out by someone who's clearly reading from a management manual.
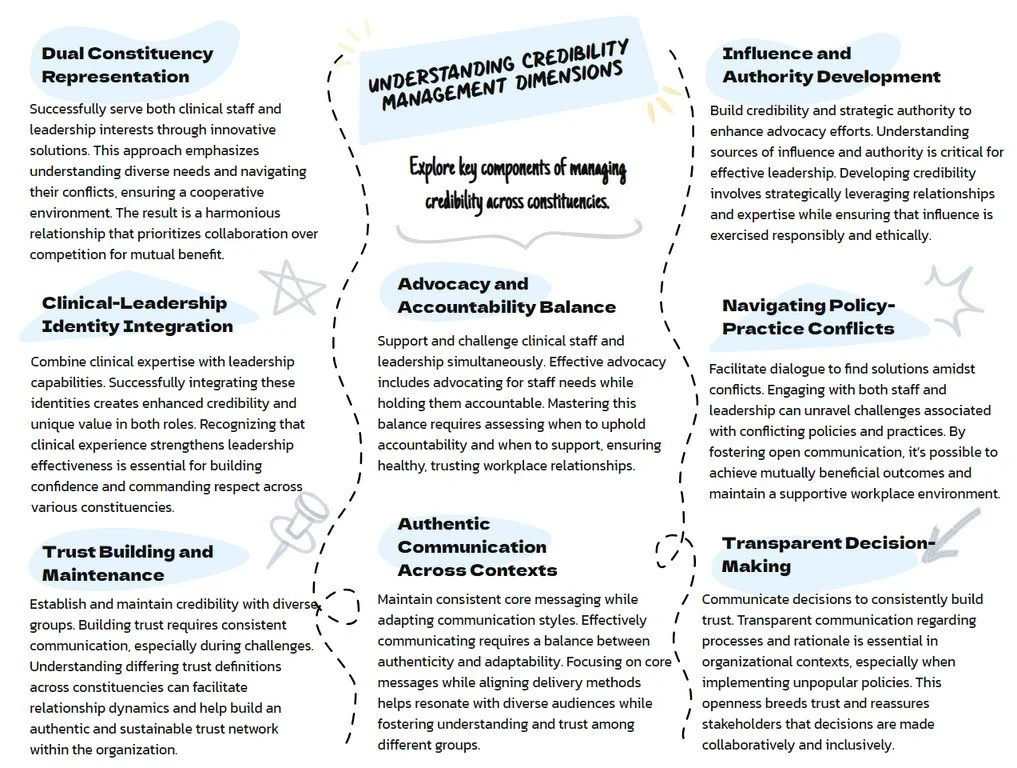
The Credibility Tightrope: Performing for Multiple Audiences
Credibility Management is perhaps the most exhausting competency of all. It's the art of maintaining trust with clinical staff (who expect you to advocate for them against "the man") while simultaneously being trusted by organizational leadership (who expect you to implement their decisions without resistance). Some days I feel like a double agent who's forgotten which side I'm supposed to be spying for.
Clinical staff watch to see if I'll "sell out" when administration asks me to implement the new productivity standards. Administration watches to see if I'm "really committed to organizational objectives" when I advocate for smaller caseloads. Meanwhile, I'm just trying to figure out how to explain to both groups that maybe, just maybe, we could find solutions that don't require anyone to compromise their professional soul or organizational survival.
Trust: The Currency That Actually Matters
Which brings me to Trust Building and Maintenance—the competency that determines whether any of this actually works. I've learned that trust isn't just about being honest and reliable (though that helps). It's about understanding that different people define trustworthiness differently. My clinical staff trust me when I understand their daily reality and advocate for their needs. My boss trusts me when I deliver results and don't surprise her with problems. The regulatory inspector trusts me when I can produce the right documentation immediately. My patients' families trust me when I return calls promptly and speak in plain English instead of clinical jargon.
The really tricky part is rebuilding trust after those inevitable moments when you mess up. Like when I promised the team we'd get new office chairs and then found out the budget had been reallocated to "essential infrastructure improvements" (which apparently means fixing the leak in the men's bathroom takes priority over our collective spinal health). Or when I had to implement a new policy that everyone hated, including me, but somehow had to present it as "an exciting opportunity for growth."
The Integration Challenge: Juggling While Riding a Unicycle
The truly exhausting part is that none of these competencies exist in isolation. I can't just be good at team building on Mondays, communication on Tuesdays, and retention on Wednesdays. Every interaction requires some combination of clinical expertise, leadership credibility, relationship management, and crisis intervention. It's like being asked to perform surgery while giving a PowerPoint presentation during a earthquake.
Some days I nail it—facilitating a difficult conversation that actually resolves a conflict, advocating successfully for a staff member's advancement, or creating a team meeting that's both productive and enjoyable. Other days I feel like I'm playing Whack-a-Mole with problems that multiply faster than I can address them, all while maintaining the professional composure that says "everything is under control" even when everything is demonstrably not under control.
The Plot Twist: It Actually Matters
Here's the thing that keeps me going despite the complexity, frustration, and occasional absurdity of it all: this work actually matters. Not just the clinical work—I knew that was important when I became a counselor. But the supervision work matters too, in ways I didn't expect.
When I help a new counselor develop confidence in their clinical skills, they become more effective with dozens of patients. When I create a team culture that supports each other through difficult cases, everyone provides better care. When I successfully advocate for resources or policy changes, it improves outcomes for every patient we serve. When I manage to retain good staff, we maintain continuity of care that can literally save lives.
The competencies outlined in these assessments aren't just professional development exercises—they're the skills that determine whether our treatment programs actually work. Whether people get the help they need. Whether families are reunited. Whether our communities become healthier and safer.
The Ongoing Journey: Embracing the Beautiful Chaos
So I continue developing these competencies, one awkward team meeting at a time, one difficult conversation at a time, one small victory at a time. I've learned that supervision excellence isn't about perfection—it's about getting incrementally better at managing the beautiful chaos that is addiction treatment while supporting the people who do this work and the people who need this work.
I assess my competencies regularly, not because I enjoy identifying my professional shortcomings (though it has become a perverse hobby), but because honest self-reflection is the only way to improve at something this complex. Each assessment reveals new patterns, new growth areas, and new ways to integrate clinical expertise with leadership responsibilities.
Some days I still miss the simplicity of individual therapy, when my biggest challenge was helping one person at a time navigate their recovery journey. But most days, I appreciate the opportunity to impact recovery outcomes on a larger scale, even if it means navigating the peculiar world where clinical excellence meets organizational management meets human resources meets regulatory compliance meets budget constraints meets staff development meets crisis intervention.
Because at the end of the day, someone has to bridge the gap between clinical expertise and organizational effectiveness. Someone has to translate between the language of patient care and the language of strategic planning. Someone has to maintain hope and motivation in a field that faces constant challenges and limited resources.
Apparently, that someone is me. And surprisingly, most days, I wouldn't trade it for anything—even a job that comes with a clear job description and functioning office chairs.
Epilogue: The Assessment Invitation
Which brings me to these competency assessments. They're not just academic exercises—they're survival tools for those of us crazy enough to believe that excellent clinical supervision can transform addiction treatment. They're roadmaps for developing the sophisticated skills required to succeed in roles that no one adequately prepared us for.
So whether you're a fellow accidental supervisor wondering how clinical skills translate to leadership effectiveness, or an aspiring supervisor trying to prepare for this beautiful chaos, or an organizational leader trying to understand why supervision development matters—these assessments offer a systematic approach to developing the competencies that actually make a difference.
Because excellent addiction treatment requires excellent clinical supervision. And excellent clinical supervision requires intentional development of skills that go far beyond clinical expertise. The patients we serve, the staff we support, and the communities we impact deserve nothing less than our commitment to continuous growth in these essential competencies.
Even if that growth happens one awkward team meeting at a time.
Clinical Leadership represents the cornerstone competency that involves integrating clinical expertise with leadership responsibilities effectively. This competency requires maintaining clinical credibility while developing the broader perspective necessary for supervision and organizational leadership. Supervisors must balance clinical expertise with leadership responsibilities, maintain credibility with both clinical staff and organizational leadership, provide clear clinical guidance while empowering staff decision-making, model evidence-based practices consistently, and integrate clinical oversight with administrative and strategic duties.
The challenge lies in the fundamental difference between clinical and leadership thinking. Clinical work focuses on individual patient care, detailed assessment, and evidence-based interventions, while leadership requires systems thinking, team dynamics management, strategic perspective, and organizational effectiveness. Many excellent clinicians struggle when promoted to supervisory positions because they lack preparation for this integration challenge, often feeling torn between their clinical identity and leadership responsibilities.