The Evolving Clinical Supervisor: Professional Development for Addiction Treatment Leaders
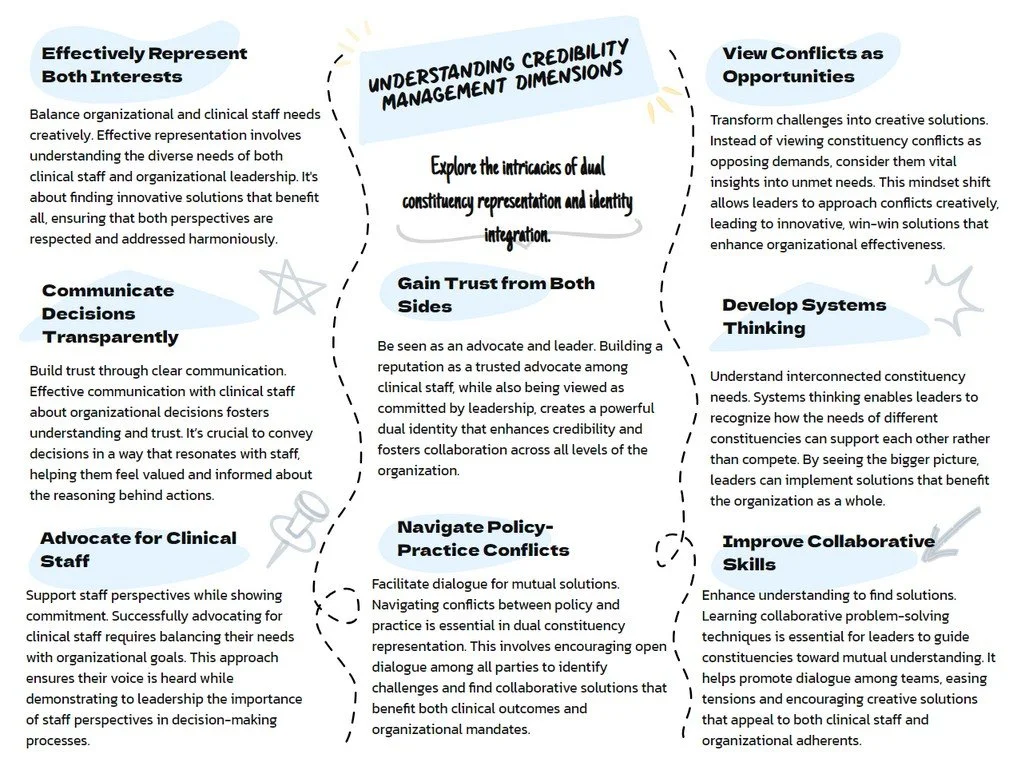
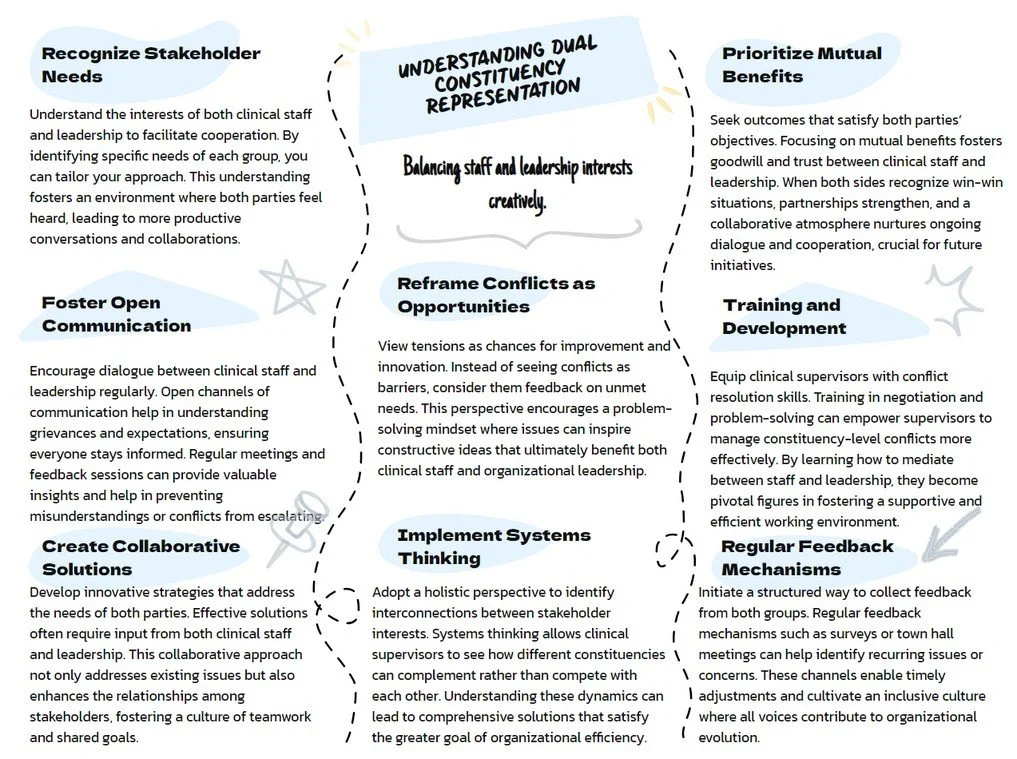
Clinical supervision in substance use disorder treatment represents one of healthcare's most challenging and impactful leadership roles. Clinical supervisors must navigate the intersection of clinical expertise and organizational responsibility while serving multiple constituencies with often competing needs and expectations. This workbook addresses the core competencies that distinguish excellent clinical supervisors from those who merely fulfill basic administrative functions.
Clinical supervisors in substance use disorder treatment face distinct pressures that set them apart from other healthcare leadership roles. They work with vulnerable populations whose lives often depend on the quality of treatment services. They supervise clinical staff who may themselves be in recovery, creating additional layers of complexity in professional relationships. They operate within regulatory environments that demand both clinical excellence and compliance with multiple oversight bodies. They must balance idealism often associated with addiction treatment with the practical realities of organizational sustainability and resource constraints.
A Clinical Supervisor's Journey: The Reality Behind the Theory
As told by someone who thought clinical supervision would be easier than this
Monday Morning: Welcome to the Impossible
So there I was, coffee in hand, looking at my calendar and wondering how I'd managed to schedule three meetings that all required me to be different versions of myself. At 9 AM, I needed to be the clinical expert advocating for evidence-based practices with my staff. At 10 AM, I was expected to be the organizational team player explaining to those same staff members why we couldn't actually implement half of those evidence-based practices due to "budget constraints" (translation: someone in accounting discovered we've been spending money on things like "adequate staffing" and "functional equipment"). By 11 AM, I'd need to transform into the competent executive who definitely wasn't having an existential crisis about whether I was a real clinician anymore or just someone who played one on TV in leadership meetings.
Welcome to what the textbooks optimistically call "dual constituency representation." I prefer to think of it as "professional schizophrenia with a side of imposter syndrome."
The Great Identity Crisis of Tuesday
Tuesday brought the delightful realization that I'd been unconsciously code-switching between my clinical and leadership personas so dramatically that I was starting to confuse myself. In the morning clinical team meeting, I caught myself using phrases like "strategic alignment" and "stakeholder engagement" when discussing treatment planning. My clinical staff looked at me like I'd started speaking ancient Sumerian.
Later, in the executive meeting, I found myself explaining budget variance analysis using addiction treatment metaphors. "Well, our Q3 spending pattern shows classic signs of fiscal relapse, with some underlying co-occurring accounting disorders that require intensive intervention..." The CFO was not amused.
This is what the experts cheerfully refer to as "clinical-leadership identity integration challenges." I call it "Wednesday is coming and I still don't know who I'm supposed to be."
The Trust Fall That Nobody Asked For
By Wednesday, I was deep into what I've come to recognize as my monthly trust crisis. You know, that special time when you realize that building trust with multiple constituencies is like trying to be everyone's favorite aunt at a family reunion where half the family is feuding and the other half is drunk.
Clinical staff want me to be their advocate—someone who fights the good fight against administrative tyranny and protects them from having to explain why they need more than seventeen minutes per patient session. Meanwhile, leadership wants me to be their reliable implementer—someone who can make unpopular decisions without causing a staff revolt or, heaven forbid, actual turnover that would require them to explain to the board why our "human capital optimization strategies" aren't working.
The really fun part is when these expectations directly contradict each other. Like when I have to explain to my clinical team that the new documentation requirements (which add approximately 847 hours to their weekly workload) are actually "quality improvements" that will "enhance patient care." The trust-building literature calls this "strategic transparency." I call it "lying with good intentions while maintaining eye contact."
Thursday: The Day Immobilization Came to Visit
Thursday was special. Thursday was the day I discovered what clinical supervision experts euphemistically call "immobilization"—that delightful state where you know exactly what needs to be done but find yourself physically incapable of doing any of it. It's like being a deer in headlights, except the deer has a master's degree and seventeen years of clinical experience.
I sat in my office, staring at a pile of performance reviews that needed to be completed, three policy drafts that required my input, and an email from HR asking why our staff satisfaction scores looked like they'd been calculated by someone having a nervous breakdown. I knew I should tackle these tasks. I wanted to tackle these tasks. I had scheduled specific times to tackle these tasks. But apparently, my brain had decided to take an unscheduled vacation to somewhere that problems don't exist and decisions aren't required.
The research calls this "action inhibition with motivational depletion." I call it "Tuesday part two: the revenge."
The really fun part about immobilization is the shame spiral that comes with it. There I was, a trained clinical professional who had helped countless clients work through their own stuck points, completely unable to apply any of those skills to my own professional paralysis. It's like being a mechanic whose car won't start because they're too exhausted to look under the hood.
Friday: The Revelation of Realistic Expectations
By Friday, I'd achieved what the literature optimistically calls "professional insight" and what I call "grudging acceptance of reality." The truth is, clinical supervision in substance use disorder treatment is inherently complicated because we're asking people to be simultaneously:
Clinical experts who stay current with evidence-based practices (because heaven knows the field changes every fifteen minutes)
Organizational leaders who can navigate budget meetings without having flashbacks to graduate school statistics courses
Staff advocates who fight for their teams (but not too hard, because that would be "problematic")
Policy implementers who can sell unpopular decisions with the enthusiasm of a used car salesman (but with more ethics and better intentions)
Trust builders who can maintain credibility with groups that define trustworthiness in completely different ways
Problem solvers who can find creative solutions to resource constraints that would make a medieval peasant weep
Mental health professionals who definitely don't need their own therapy (spoiler alert: we do)
The beautiful irony is that we work in addiction treatment—a field dedicated to helping people recognize that recovery is an ongoing process requiring daily attention, support systems, and acceptance of imperfection—while somehow expecting ourselves to achieve professional perfection without similar supports or patience.
The Weekend Reflection: Competencies and Caffeine
So here I am, Saturday morning, writing this while consuming what might be my fourteenth cup of coffee this week, reflecting on what I've learned about the glamorous world of clinical supervision competencies.
Credibility Management isn't really about being credible—it's about being credible to multiple audiences simultaneously, each of whom has different definitions of what credibility looks like. It's like being asked to perform Shakespeare for a crowd that includes both literary scholars and people who think the Bard is that guy from Game of Thrones.
Trust Building isn't about being trustworthy—it's about being trustworthy in ways that make sense to people who may have completely different values, priorities, and definitions of reliability. It's like being asked to be everyone's best friend at a party where you don't know anyone and half the guests are having philosophical disagreements about the nature of friendship itself.
Identity Integration isn't about having a professional identity—it's about having multiple professional identities that somehow need to coexist in the same body without causing psychological whiplash. It's like being asked to be a Swiss Army knife, except each tool needs to be sharp enough for precision work while somehow still fitting in the same compact space.
Immobilization Recognition isn't about not getting stuck—it's about recognizing when you're stuck and having strategies for getting unstuck that don't involve hiding under your desk until the problems solve themselves (which, despite extensive testing, appears to be an ineffective approach).
The Monday Morning Epilogue: Armed with Self-Awareness
As I prepare for another week of clinical supervision adventures, I'm armed with something I didn't have before: the recognition that this work is supposed to be complicated. The challenges aren't signs that I'm failing at supervision—they're signs that I'm doing supervision in a complex environment that requires sophisticated skills.
The assessments and frameworks aren't magic solutions that will eliminate all supervisory challenges. They're more like GPS systems—they help you figure out where you are, where you're trying to go, and suggest some routes that might work better than driving around in circles while muttering about how things used to be simpler.
Will I still have days when I question whether I'm cut out for this work? Absolutely. Will I still find myself caught between competing constituency demands while experiencing minor identity crises? Without a doubt. Will I occasionally find myself immobilized by the sheer complexity of trying to be all things to all people while maintaining my sanity and at least some professional dignity? Signs point to yes.
But now I have language for these experiences. I have frameworks for understanding them. I have strategies for working through them. And perhaps most importantly, I have the recognition that these challenges are normal parts of clinical supervision rather than personal failings requiring immediate career changes or extensive therapy (though the therapy is still probably a good idea).
The work continues. The coffee remains essential. And somewhere between the dual constituency demands and the identity integration challenges, actual supervision happens—imperfect, complicated, occasionally frustrating, but ultimately meaningful supervision that helps both staff and patients navigate their own complex journeys.
After all, if recovery is a process rather than a destination, maybe supervisory excellence is too. And if that's the case, I'm exactly where I'm supposed to be: somewhere in the middle of figuring it out, armed with better maps and a stronger appreciation for the terrain.
Now, if someone could just explain to me why we need seventeen different forms to document a single supervision session, I'd really appreciate it.